ELSA ZERBINI ¹, ADRIANA GRECO ², SILVIA ESTRADA 4 , MARIO CISNEROS ³, CARLOS COLOMBO 5 ,
SOLEDAD BELTRAME ², CARINA BONCOMPAIN 6 , SEBASTIÁN GENERO 7
¹ Instituto Nacional de Enfermedades Respiratorias Dr. Emilio Coni (ANLIS Malbrán), Santa Fe, ² Programa Nacional de Control de Tuberculosis – Argentina, ³ Programa de Tuberculosis – Jujuy, 4 Programa de Tuberculosis – Salta, 5 Programa de Tuberculosis – Formosa, 6 Programa de Tuberculosis – Santa Fe, 7 Programa de Tuberculosis – Chaco, Argentina
Abstract Tuberculosis (TB) remains a cause of illness and death across the world, especially in developing
countries and vulnerable population groups. In 2013, 1.5 million died from the disease worldwide. In Argentina, the largest proportion of TB-related deaths occurred in the northern provinces. Several international studies reported that TB mortality was related to the presence of certain comorbidities and socio-demographic characteristics. Our aim was to investigate the main risk factors associated with TB mortality in adults from six provinces in Argentina, especially those with higher TB mortality rates. A retrospective case-control study was conducted. It included all patients of ≥18 years with clinical and/or bacteriological TB diagnosis who underwent treatment from January 1st, 2012 to June 30th, 2013. Socio-demographic, clinical and bacteriological variables were surveyed. Information on 157 cases and 281 controls was obtained. Patients reported as deceased to the TB Control Program were considered cases, and those whose treatment result was reported as successful in the same time period were considered controls. For 111 deaths, the average time elapsed between the start of treatment and death was 2.3 months; median: 1. TB-related mortality was associated with poor TB treatment adherence (OR: 3.7 [1.9-7.3], p: 0.000), AIDS (OR: 5.29 [2.6-10.7], p: 0.000), male gender (OR: 1.7 [1.1-2.5], p: 0.009), belonging to indigenous people (OR: 7.2 [2.8-18.9], p:0. 000) and age ≥ 50 (OR: 2.2 [1.4-3.3], p: 0.000). By multivariate analysis the two first associations were confirmed. This study sets up the basis for planning inter-program and inter-sector work to accelerate the decline in the inequitable TB mortality.
Key words: tuberculosis, mortality, epidemiology, comorbidities, sociodemographic factors
Resumen Factores de riesgo asociados con la mortalidad por tuberculosis en adultos de seis provincias
de Argentina. En 2013, 1.5 millones de personas murieron por tuberculosis (TB) en el mundo, especialmente en países en desarrollo y grupos de población vulnerables. En Argentina, la mayor proporción de muertes asociadas con TB ocurrió en las provincias del norte. Estudios internacionales observaron que la mortalidad por TB estaba relacionada con comorbilidades y características sociodemográficas. Este estudio pretendió investigar cuáles eran los principales factores de riesgo asociados con la mortalidad por TB en adultos de seis provincias argentinas, especialmente aquellas con mayores tasas de mortalidad por TB. Se realizó un estudio retrospectivo casos-controles, incluyendo todos los pacientes ≥ 18 años con diagnóstico clínico y/o bacteriológico de TB en tratamiento entre el 1° de enero de 2012 y el 30 de junio de 2013. Se obtuvo información de 157 casos y 281 controles, considerándose casos los pacientes notificados como fallecidos al Programa de TB y controles aquellos cuyo resultado de tratamiento fue notificado como éxito o curado en el mismo período de tiempo. El tiempo transcurrido entre el comienzo del tratamiento y la muerte fue 2.3 meses; mediana: 1. Las muertes relacionadas con TB estuvieron asociadas con: escasa adherencia al tratamiento (OR: 3.7 [1.9-7.3], p: 0.000), sida (OR: 5.29 [2.6-10.7], p: 0.000), género masculino (OR: 1.7 [1.1-2.5], p: 0.009), pertenencia a pueblos originarios (OR: 7.2 [2.8-18.9], p: 0.000) y edad ≥ 50 (OR: 2.2 [1.4-3.3], p: 0.000). Por análisis multivariado, se confirmaron las dos primeras asociaciones. Este estudio sienta las bases para planificar acciones destinadas a acelerar el descenso de la mortalidad por TB.
Palabras clave: tuberculosis, epidemiología, mortalidad, comorbilidades, factores sociodemográficos
Received: 22-IX-2016 Accepted: 19-X-2016
Postal address: MSc. Elsa Zerbini, Instituto Nacional de Enfermedades Respiratorias Dr. Emilio Coni, ANLIS Malbrán, Blas Parera 8260, 3000 Santa Fe, Argentina
e-mail: elsazerbini@arnet.com.ar
Although there is a cost-effective treatment, tuberculosis (TB) remains a cause of illness and death across the world, especially in developing countries and the most vulnerable population groups. In 2014, 9.6 million new TB cases were estimated and 1.5 million died from the disease worldwide1.
In Argentina, the TB case reported rate in 2014 was 24.7 per 100 000 inhabitants, with 9605 new cases2. There was an increase in the TB notification rate of 5.1% from the previous year, and a tendency toward stability was observed in the TB death rate, with a record of 1.60 deaths per 100 000 people in 20142, 3. More than one third of the TB-related deaths between 35 and 44 years were associated with the Human Immunodeficiency Virus (HIV) infection and 46.9% were younger than 55 years, including economically active age groups3. The largest proportion of TB-related deaths in the biennium 2012-2013 occurred in the northern provinces of the country, with rates nearly 5 times higher than the average for Argentina (1.63 per 100 000)3. The highest mortality rates were those from Jujuy, Formosa, Chaco and Salta, which were 8.4, 7.7, 4.5 and 3.8 per 100 000 respectively. This shows that mortality from this disease is a serious public health problem, especially in provinces from the north of Argentina which have the highest proportion of population with unsatisfied basic needs4.
Several studies reported that TB mortality was closely related to the presence of certain comorbidities (HIV/AIDS, among others) and certain socio-demographic patient characteristics and living features5-14. TB mortality tends to be higher in the first two months of TB treatment and early mortality increases in specific patient-groups, including elderly people and those with previous TB episodes, smear-negative TB and extra-pulmonary TB. HIV co-infection increases the TB mortality rate, and HIV-positive patients continue to die throughout TB treatment, whereas mortality in HIV-negative patients declines rapidly after the first month of treatment15, 16. Given the wide range of results and the need to set events in context for decision-making, this study aims to investigate which are the main risk factors associated with TB mortality in six provinces of Argentina, especially those with higher TB mortality rates.
Materials and methods
A retrospective case-control study was conducted in the provinces of Jujuy, Formosa, Chaco, Salta, Neuquén and Santa Fe, where mortality rates in 2012-2013 biennium were 8.36; 7.69; 4.50; 3.85; 1.43 and 0.92 per 100 000 inhabitants respectively17. In the same provinces, TB lethality rates were 13.4; 10.5; 5.8; 11.3; 1.0 and 6.1 per cent respectively. The first four provinces were chosen for their high mortality rates and the last two for convenience. It included all patients of ≥ 18 years, new cases and those with a history of previous treatment, patients with clinical and/or bacteriological TB diagnosis, sensitive or resistant to TB drugs, with pulmonary and/or extra-pulmonary TB, who underwent treatment in the period from January 1st 2012 to June 30th 2013.
TB patients reported as deceased to the TB Control Program (TBCP) in the aforesaid period were considered cases, and those whose treatment result was reported as successful to the TBCP (i.e., cured or with completed treatment according to national technical standards) in the same period of time were considered controls.
Based on the reported death count for the period under study, a sample size of 158 cases and 316 controls was estimated using EPI-DAT software, with a confidence interval of 95% and a power of 80%.
Sociodemographic, clinical and bacteriological variables were surveyed. For the “indigenous people” variable, the definition by the “Instituto Nacional de Estadísticas y Censos” (INDEC) was taken18. To identify the native population, the statement of the interviewees (relatives of the deceased or patients in the case of controls) were respected and combined two criteria: self-identification and self-recognition of belonging to an indigenous people and indigenous descent in first generation.
TB treatment adherence was defined as the degree of compliance in taking the drug doses specified in each phase of treatment. Those patients who took the recommended doses were considered adherents.
For data collection, clinical history and treatment cards were examined from cases and controls under study, and TB National and Provincial Control Programs databases. A data collection and registry form was drafted, with its layout based on the previously considered variables. A pilot test for the collection instruments was performed with 10 cases and 10 controls. Researchers agreed to take precautions to protect the privacy and confidentiality of the data collected, as specified in the National Law 25 326 of Habeas Data, omitting information that would identify patients and limiting access only to those data directly involved in the present study.
Data analysis was conducted using Epi Info software version 3.5.1. Patient characteristics were recorded using the mean, median and range for continuous variables. To evaluate the association between the characteristics of TB patients and the risk for mortality, univariate analysis was performed; the chi-squared test or Fisher’s exact test were used for the categorical variables. The variables with < 0.10 in the univariate analysis were included in a multivariate logistic regression model. A < 0.05 was considered statistically significant. The strength of association was determined by calculating odds ratios (OR) and their 95% confidence intervals (CIs).
The approval from the “Health Investigation Committee” of the National Ministry of Health, which analyzes ethical aspects, was obtained on March, 2013.
Results
Information on 157 cases and 281 controls was obtained. However, not for all the information could be obtained in every variable. In Table 1, the main characteristics of TB deceased cases are displayed. Among all 41 deceased cases of whom information about drug addiction could be obtained, 4 (9.8%) were addicted and 3 of them had AIDS.
For 111 deaths of which the decease date was available, the average time elapsing between the start of treatment and decease was 2.3 months (range: 0-6), the median was 1, the mode 0 (considering 0 those who died before the first month), and percentiles 25% and 75%, 0.5 and 2 respectively. Forty per cent died before reaching the first month of treatment, and 63% before reaching the second month.
Of all 44 patients known to have died before the first month of treatment, 70% were male, 41% were 65 years of age or older, 58% were unmarried or without a partner, 100% had pathological radiology, 91% had pulmonary TB, 78% were bacteriologically confirmed through direct examination, 7% had a history of prior treatment and 11% had AIDS.
Of all 30 patients known to have died from AIDS/TB association, 79% were between 18 and 49 years old and
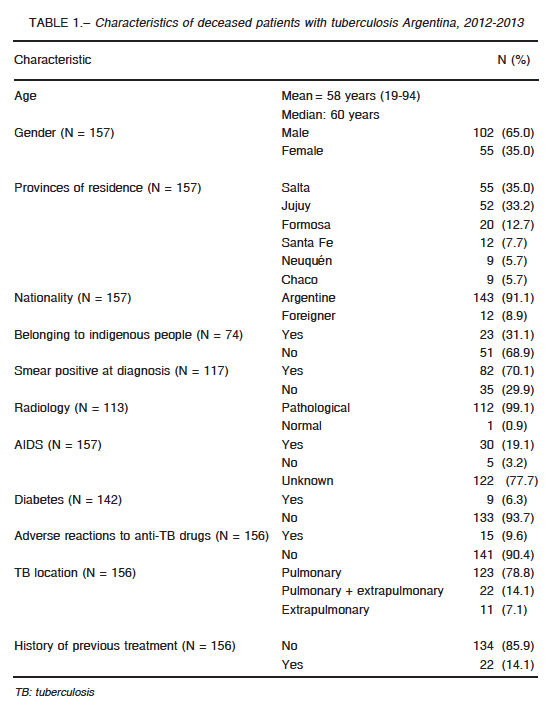
93% had a pulmonary presentation of TB. Of all 28 cases with pulmonary TB, 10 also had extrapulmonary location.
A statistically significant association was observed between TB-related mortality and poor TB treatment adherence, male gender, presence of AIDS, belonging to indigenous people and age over 50. In Table 2, results of the univariate analysis are presented, where only the most relevant and/or prevalent associations were considered.
No statistically significant association was observed between mortality and presence of adverse reactions to anti-TB drugs (ARADs). However, in considering specifically the province of Jujuy where the highest proportion of ARADs was reported, it is clear that ARADs occurred for the most part in patients who died than in those who did not [OR: 4.9 (1.6-15.1), p: 0.033]. In this province, among 52 cases and 109 controls, a statistically significant association was observed between presence of anemia and TB-related death [OR: 2.4 (1.2-4.6), p: 0.006].
AIDS-associated TB-related deaths were more frequent in men than in women [OR: 2.3 (0.9-5.4), p: 0.03].
Among the other reported pathologies and addictions to exceed a 5% percentage considering the total number of deaths (157), other infectious conditions (5.1%) and kidney conditions (5.1%) were found. Nevertheless, they did not prove to be associated with TB mortality.
Deaths occurring prior to the first month of treatment were significantly associated with the fact of patients being single or without a partner [OR: 3.0 (1.1-8.8),
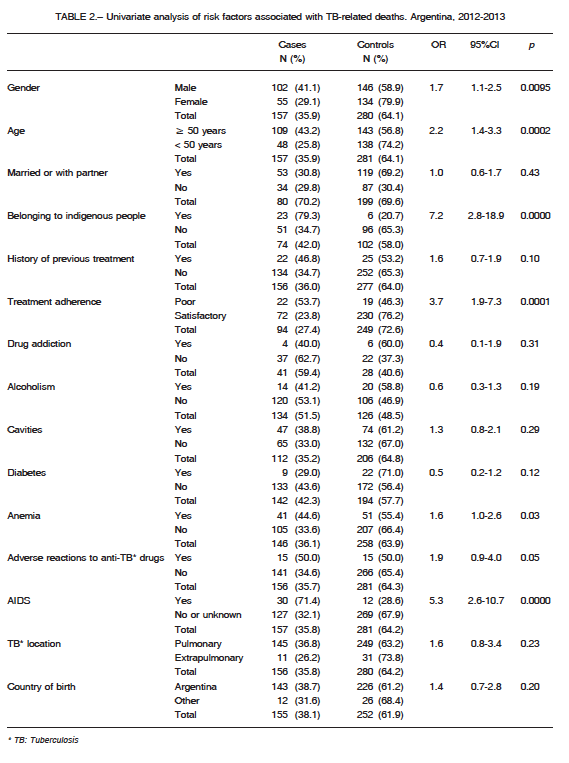
p:0.02]. These deaths were also associated, though not significantly, with sputum smear positive diagnosis [OR: 1.4 (0.5-3.5), p: 0.25].
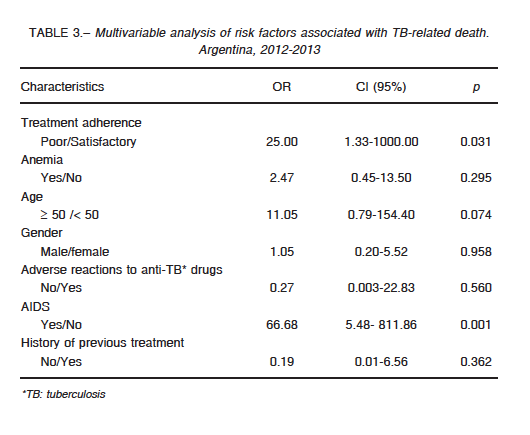
In Table 3, results of the multivariate analysis can be observed. The variables that remained significant risk factors for death were poor TB treatment adherence [OR: 25.0 (1.3-1 000.0), p: 0.03] and AIDS [OR: 66.7 (5.48-811.9), p: 0.001]. A major limitation for multivariate analysis was that it could only be performed for 74 patients who had the information of all the selected variables to analyze. The variable “indigenous peoples” could not be included in the multivariate analysis because of incomplete information.
Discussion
Although studies have been developed in Argentina analyzing TB mortality, to our knowledge there is no record that any such studies had been designed specifically to analyze risk factors associated with TB mortality. The main limitation of this study is its retrospective nature, which made it necessary to use primary sources, such as generally incomplete medical records and treatment cards.
Deceased patients were mostly Argentinean and males, with an average age of 58; 93% of them were pulmonary TB cases, 18% of whom had also an extra-pulmonary TB localization and 9.6% presented ARADs. Nineteen per cent of those patients that were tested for HIV presented TB/AIDS association. In a study by Kim et al. the the average age of death was 10 years older than here, what seems more consistent for a developed country19; in this study most of deceased cases were also males and 84% had positive sputum smear tests, higher than in our study, where it only achieved 70%.
Field et al., like us, also found a high mortality in the first month after starting TB treatment in new cases as well as in retreated cases15. They suggest that TB prevention and early accurate diagnosis, recognition of the role of HIV and shorter pathways to TB treatment initiation may reduce death rates. This early lethality may be related to excessive TB diagnosis delay, as noticed in an earlier study in Argentina in which two of the provinces involved in this investigation participated20.
From predicting factors of TB-related deaths, from which good information coverage could be attained, a statistically significant association was observed for male gender, age older than or equal to 50, poor adherence to TB treatment and AIDS. Indigenous origin also resulted statistically significant, but the validity of this result was limited by the low information coverage. Male gender was mentioned as a risk factor in many studies; Kwon et al. add that differences between males and females, just like adherence in treatment, alcohol abuse, smoking behavior, and use of health services might explain this result21. In this work the same type of association could not be verified. Although an increased death risk was observed in non-foreign patients, those with a history of prior TB treatment, those who suffered from ARADs, or presented lung cavities, anemia, or pulmonary TB location, these results did not reach statistical significance. A history of previous treatment, non-foreign condition and ARADs were also mentioned as risk factors for TB mortality in a study conducted in Iran22. Kim et al. in Korea found a significant association between TB mortality and
anemia, and also positive sputum smear result at the time of diagnosis, and did not find any association with the presence of diabetes disease19.
TB is known to be the most common associated infection and the leading cause of death in HIV patients worldwide, especially in limited-resource settings; it is not surprising that in this study, AIDS was one of the main risk factors of TB-related death1, 23. In a study conducted in North Carolina, US, over a 10-year period (1993-2003), risk factors for TB-related death included old age, miliary or meningeal diseases and HIV24. In other study conducted in San Francisco, California, US, Nahid et al. reported factors for TB-related death such as HIV infection, old age, positive sputum smear result, and poor TB treatment courses25.
For health policy makers, it is important to reinforce training of health personnel on TB/HIV co-infection diagnosis and management, making TB and HIV drugs and cotrimoxazole consistently available to anyone requiring them in order to avoid stock-outs, and strengthening TB and HIV treatment collaborative activities in order to generate the expertise needed for a well coordinated joint approach to care of TB/HIV co-infected patients.
Waitt et al. in a systematic review conducted in 2011, pointed to the TB/HIV association as a death predictor in patients treated for TB in two countries in America: Brazil and Peru16; the strength of association in the two studies from Brazil is similar to that of Argentina, while in Peru, a country with high TB rate, it is much higher26-28.
Nahid et al. found that the association between treatment interruption and risk of death was due to poor adherence during the intensive phase of treatment25. In this study, poor adherence to TB treatment was four times larger in patients who died than in those who did not.
The low number of other comorbidities very likely was related to shortcomings in records, as well as lack of time to investigate, since about half of patients died before completing the first month of treatment.
A fact that should not be overlooked is the association between mortality and indigenous origin, as this would point to other sociodemographic, economic and cultural factors characteristic of these people, such as unfavorable housing conditions in confined areas with poor ventilation and poor sanitation. Other relevant factors include migration from rural to urban areas and sociocultural characteristics associated with a different health-illness-healing pattern than the rest of the population besides a lack of proper cultural adjustment of services and problems in health care organization. In Chile, this was evidenced by CEPAL in a study conducted in 2007, where relative risks of dying from TB proved to be between 2.9 and 6.5 times higher in indigenous in relation to non-indigenous populations29. In Peru, a high rate of TB occurrence have been reported in indigenous population, further and deeper research being recommended in order to produce more reliable evidence about the situation of TB in this population; this may also be recommended in Argentina, as there is no such information available30.
Despite the problems of lack of information, mentioned in the study, which limited the scope of the multivariate analysis, in the latter it was concluded that AIDS and poor TB treatment adherence are significantly associated with TB-related death, which confirms the relevance of these two risk factors.
In conclusion, this study can provide a good basis for planning inter-program and inter-sector work to accelerate the decline in the inequitable TB mortality, especially strengthening strategies that support control of TB/HIV co-infection and adherence to TB treatment. Thus, it will contribute to the End TB Strategy success whose goal for 2020 is to have reduced the number of TB deaths by 35% compared to 201531.
Acknowledgements: To the Comisión Nacional de Investigación en Salud, Ministerio de Salud de Argentina for funding six scholarships for professionals to perform the fieldwork.
Conflict of interests: None to declare
References
1. World Health Organization (WHO). Global Tuberculosis Report 2015. Geneva: WHO; 2015. In: http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf; accessed on 8/10/2016.
2. Instituto Nacional de Enfermedades Respiratorias (INER). Notificación de casos de tuberculosis en la República Argentina. Período 1985-2014. Santa Fe, Argentina: INER; 2016. In: http://www.anlis.gov.ar/iner/wp-content/uploads/2016/04/Notificaci%C3%B3n-de-Casos-de-TB-en-la-Rep%C3%BAblica-Argentina-2014.pdf; accessed on 8/10/2016.
3. Instituto Nacional de Enfermedades Respiratorias (INER). Mortalidad por tuberculosis en Argentina, 1980-2014. Santa Fe, Argentina: INER; 2016. In: http://www.anlis.gov.ar/iner/wp-content/uploads/2016/04/BoletinActualizacionMortalidadTuberculosisDocTec0316.pdf; accessed on: 8/10/2016.
4. Instituto Nacional de Estadísticas y Censos (INDEC). Censo Nacional de Población, Hogares y Viviendas 2010. Buenos Aires, Argentina: INDEC; 2010. In: http://www.censo2010.indec.gov.ar/cuadrosDefinitivos/indice_de_cuadros.pdf.; accessed on 14/9/2016.
5. Churchyard GJ, Kleinschmidt I, Corbett EL, Murray J, Smit J, De Cock KM. Factors associated with an increased case-fatality rate in HIV-infected and non-infected South African gold miners with pulmonary tuberculosis. Int J Tuberc Lung Dis 2000; 4: 705-12.
6. Mathew TA, Ovsyanikova TN, Shin SS, et al. Causes of death during treatment in Tomsk Oblast, Russia. Int J Tuberc Lung Dis 2006; 10: 857-63.
7. Caylà JA, Rodrigo T, Ruiz-Manzano J, et al. Tuberculosis treatment adherence and fatality in Spain. Respiratory Research 2009; 10: 121.
8. Gadkowski LB, Hamilton CD, Allen M, et al. HIV-specific health care utilization and mortality among tuberculosis/HIV coinfected persons. AIDS Patient Care and STDS 2009; 23: 845-51.
9. Jung R, Bennion JR, Sorvillo F, Bellomy A. Trends in tuberculosis mortality in the United States, 1990-2006: A population-based case-control study. Public Health Reports 2010; 125: 389-97.
10. Santos Junior JDO, Pereira BB. Dynamic study of tuberculosis mortality in Sao Paulo State, Brazil: a Bayesian approach. Cad Saúde Pública 2011; 27: 1415-22.
11. Feng J Y, Su WJ, Chiu YC, et al. Initial presentations predict mortality in pulmonary tuberculosis patients. A prospective observational Study. PLoS ONE 2011; 6: e23715.
12. Yen YF, Rodwell TC, Yen MY, et al. DOT associated with reduced all-cause mortality among tuberculosis patients in Taipei, Taiwan, 2006-2008. Int J Tuberc Lung Dis 2012; 16: 178-84.
13. Kayigamba FR, Bakker MI, Mugisha V, et al. Adherence to tuberculosis treatment, sputum smear conversion and mortality. PLoS ONE 2013; 8: e73501.
14. Lin CH, Lin CJ, Kuo YM, et al. Tuberculosis mortality: Patient characteristics and causes. BMC Infect Dis 2014; 14: 5.
15. Field N, Lim M, Murray J, Dowdeswell R, Glynn J, Sonnemberg P. Timing, rates, and causes of death in a large South African tuberculosis programme. BMC Infect Dis 2014; 14: 3858.
16. Waitt CJ, Squire SB. A systematic review of risk factors for death in adults during and after tuberculosis treatment. Int J Tuberc Lung Dis 2011; 15: 871-85.
17. Instituto Nacional de Enfermedades Respiratorias (INER). Mortalidad por Tuberculosis en la República Argentina. Período 1980-2013. Santa Fe, Argentina: INER; 2015. In: http://www.anlis.gov.ar/iner/wpcontent/uploads/2014/02/MortalidadTB2013_web_24112015.pdf; accessed on 14/9/2016.
18. Instituto Nacional de Estadísticas y Censos (INDEC). Encuesta Complementaria de Pueblos Indígenas 2004-2005. In: http://www.indec.gov.ar/micro_sitios/webcenso/ECPI/index_ecpi.asp.; accessed on 9/10/2016.
19. Kim CW, Kim S, Lee SN, et al. Risk factors related with mortality in patient with pulmonary tuberculosis. Tuberc Respir Dis 2012; 73: 38-47.
20. Zerbini E, Chirico MC, Salvadores B, Amigot B, Estrada S, Algorry G. Delay in tuberculosis diagnosis and treatment in four provinces of Argentina. Int J Tuberc Lung Dis 2008; 12: 63-8.
21. Kwon YS, Kim Y, Song JU, et al. Factors for death during pulmonary tuberculosis treatment in Korea: A Multicenter Retrospective Cohort Study. J Korean Med Sci 2014; 29: 1226-31.
22. Alavi Naini R, Moghtaderi A, Metanat M, Mohammadi M, Zabetian M. Factors associated with mortality in tuberculosis patients. J Res Med Sci 2013; 18: 52-5.
23. Agbor AA, Bigna JJR, Billong SC, et al. Factors associated with death during tuberculosis treatment of patients co-infected with HIV at the Yaoundé Central Hospital, Cameroon: An 8-year retrospective cohort study (2006-2013). PLoS ONE 2014; 9: e115211.
24. Nguyen LT, Hamilton CD, Xia Q, Stout Je. Mortality before or during treatment among tuberculosis patients in North Carolina, 1993-2003. Int J Tuberc Lung Dis 2011; 15: 257-62.
25. Nahid P, Jarlsberg L, Rudoy I, et al. Factors associated with mortality in patients with drug-susceptible pulmonary tuberculosis. BMC Infect Dis 2011; 11: 1.
26. Pessoa Militao De Albuquerque MF, Arraes de Alencar Ximenes R, Lucena-Silva N, et al. Factors associated with treatment failure, dropout, and death in a cohort of tuberculosis patients in Recife, Pernambuco State, Brazil. Cad Saúde Pública 2007; 23: 1573-82.
27. Pereira Domingos M, Teixeira Caiaffa W, Colosimo EA. Mortality, TB/HIV co-infection, and treatment dropout: predictors of tuberculosis prognosis in Recife, Pernambuco State, Brazil. Cad Saúde Pública 2008; 24: 887-96.
28. Kawai V, Soto G, Gilman R, et al. Tuberculosis mortality, drug resistance, and infectiousness in patients with and without HIV infection in Peru. Am J Trop Med Hyg 2006; 75: 1027-33.
29. Pedrero MM, Oyarce AM. Una metodología innovadora para la caracterización de la situación de salud de las poblaciones indígenas de Chile: limitaciones y potencialidades. Notas de Población-CEPAL 2009; 89: 119-45.
30. Culqui D, Trujillo O, Cueva N, Aylas R, Salaverry O, Bonilla C. Tuberculosis en la población indígena del Perú 2008. Rev Peru Med Exp Salud Publica 2010; 27: 8-15.
31. World Health Organization (WHO). The End TB Strategy. Ginebra, Suiza: WHO; 2015. In: http://www.who.int/tb/post2015_TBstrategy.pdf?ua=1; accessed on 14/9/2016.
– – – –
Y a los arbitristas y reformadores de oficio convendría advertirles:
Primero: Que muchas cosas que están mal por fuera están bien por dentro.
Segundo: Que lo contrario también es frecuente.
Tercero: Que no basta mover para renovar.
Cuarto: Que no basta renovar para mejorar.
Quinto: Que no hay nada que no sea absolutamente empeorable.
Antonio Machado (1873-1939)
Juan de Mairena I. Sentencias, donaires, apuntes y recuerdos de un profesor apócrifo. Cuarta edición. Buenos Aires: Losada, 1968, p 19
