GABRIELA V. CARRO, ELSA M. CARLUCCI, IVAN TORTEROLA, PABLO BREPPE, MIGUEL ÁNGEL TICONA ORTIZ, JAVIER E. PALOMINO PALLAREZ
Unidad de Pie Diabético, Hospital Nacional Profesor Alejandro Posadas, Buenos Aires, Argentina
Resumen: A fines de 2019 se identificó un nuevo coronavirus como causa de neumonía, en Wuhan, China. Esta nueva enfermedad (COVID-19) causó un inesperado vuelco en la economía y en la sociedad. El aislamiento social y el confinamiento provocaron cambios en la dinámica de las consultas médicas. En este estudio se compararon la cantidad de consultas y la gravedad de las lesiones nuevas en la Unidad de Pie Diabético entre junio de 2020 y junio de 2019. Se analizaron en total 356 visitas médicas, hallando un 29% de reducción en el número de visitas en 2020. El número de consultas por lesión nueva aumentó del 6.4% a 10.3% (p = ns) durante la pandemia. Las visitas de familiares por diversos motivos en lugar del paciente aumentaron durante 2020 de 1.4% a 16.3% (p < 0.05). Los controles de pacientes sin lesión (pie de alto riesgo, control post alta), disminuyeron de 16.8% a 4.5% (p < 0.05) y también aumentaron las visitas únicamente para prescripciones médicas (7.3% a 22.4%, p < 0.05). En nuestra muestra, no hubo diferencias significativas en la gravedad de la presentación ni en los días de evolución de las lesiones nuevas en relación al año anterior. Durante 2020 las teleconsultas representaron el 7% del total. En junio de 2019 no se registraron amputaciones mayores y en 2020 se registraron 4. Dada la dinámica del confinamiento, se requiere un continuo seguimiento y nuevos estudios para evaluar las consecuencias que se producirán en los pacientes con esta enfermedad con el fin de tomar decisiones acertadas.
Palabras clave: pie diabético, COVID-19, consultas médicas
Abstract At the end of 2019 a novel coronavirus was identified as a cause of pneumonia in Wuhan, China. This emerging disease has caused an unexpected turn in the economy and in society, which has led to the necessity of social isolation and confinement. Diabetic foot consultation was affected by the ongoing situation. The aim of this study was to compare the number of medical visits and the severity of new lesions at presentation at the Diabetic Foot Unit during June 2020 compared to June 2019. Three hundred and fifty six medical visits were analyzed, resulting in a 29% reduction in the number of visits during 2020. The number of patients presenting with new lesions increased from 6.4% to 10.3% (p = ns) during pandemic. The number of visits from the patients´ relatives was higher during June 2020 (16.3% vs. 1.4%) (p < 0.05). Controls of feet without active lesions (i.e.: closed wound or periodic control) decreased from 16.8% to 4.5% (p < 0.05). Consultation for medical prescription only was higher in 2020 (22.4%) than in 2019 (7.3%) (p < 0.05). In our sample, there were no significant differences in the severity of new lesions at presentation or on the days of evolution of new ones in comparison with the previous year. During 2020, telehealth consults represented a 7% of all medical visits. There were no major amputations during 2019 and 4 during 2020. Given the dynamics of confinement, further studies about this topic are required to make sound and accurate decisions.
Key words: diabetic foot, COVID-19, medical consultation
Postal address: Gabriela Carro, Maison 769, 1712 Castelar, Buenos Aires, Argentina
e-mail: gabivcarro@yahoo.com.ar
• During COVID-19 outbreak, health systems had to be reorganized in order to meet the new necessities. Guidelines on diabetic foot practice gave advice on how to treat this pathology but not many studies were carried out on this topic.
• This study shows changes in medical consultation in a diabetic foot unit early in COVID-19 pandemic, comparing data from 2019 and 2020. There was a 29% reduction in medical visits, augment in patients‘ relatives consultation, higher rates of major amputation and little changes in consultation for new lesions.
At the end of 2019 a new coronavirus was identified as a cause of pneumonia, in Wuhan, China. It quickly spread to other countries around the globe, and became the cause of an epidemic in China and a pandemic a few months later. The disease was called COVID-19 as defined by the World Health Organization (WHO) 1, 2. This emerging disease has caused an unexpected turn in the economy and in society in the whole world and made health systems collapse in a few weeks. It has also led to the necessity of social isolation to avoid a large number of deaths. Consequences were devastating for population and economy, and health systems had to be reorganized in order to meet the new emerging necessities caused by this novel disease, avoiding the collapse of medical attention. At this moment, in our country there is a growing demand of health services but health system has not collapsed yet. Positive case curves are increasingly rising and that is the reason why people are advised to stay at home and self-isolate 3 in a mandatory quarantine since March 20th. The number of medical visits dropped to less than a half early in quarantine, and consultation was limited to severe and urgent pathologies, leaving patients at high risk of reulceration 4 without checkups.
In the case of diabetic foot, there are certain conditions such as diabetic foot attack 5, which require urgent treatment, and others not so severe but dangerous enough to require some kind of control. Patients with lesions in the latter case were not consulting at this time. However, as time went by, diabetic foot consultation started rising.
There are some assumptions about the outcomes of the diabetic foot during pandemic. Some argue that patients consult late in the course of a diabetic foot and present with more severe lesions. On the other hand, quarantine warrants repose, and this might help patients to avoid walking and allow them to off-load diabetic foot ulcers, leading to the improvement of the lesions. Other concerns arise as to the potential relationship between COVID-19 and diabetic foot regarding ischemia, neuropathy and cytokine alterations 6. At present there is little evidence about diabetic foot outcomes during pandemic. The purpose of this study was to compare the number of medical visits and the severity of lesions at presentation at the diabetic foot unit during June 2020 in relation to June 2019 after 70 days of social isolation with 17 415 confirmed cases and 539 deaths because of COVID-19.
Materials and methods
This is a cross sectional study. During June 2020, patients older than 18 years that consulted to Diabetic Foot Unit in Hospital Nacional Prof. A Posadas for any reason (diabetic foot control, development of new lesions, medical prescriptions, periodic control of foot with previous lesions) were prospectively included and enrolled in a prospective database and the information was compared to that of patients that consulted in June 2019 whose data were obtained from medical records and statistical database made for statistical purposes. Data on number of visits, reasons for the visit and characteristics of new lesions were analyzed. The investigators assessed the severity of the new lesions using Saint Elian 7, WIfI 8 and Texas 9 classifications. Peripheral arterial disease was assessed by the palpation of pulses and by ABI index, which was measured using a portable duplex ultrasound Contec with an 8 MHz probe. Neuropathy was evaluated to calculate Saint Elian score, determining loss of protective sensation by Ipswich touch test. Saint Elian classification was calculated according to the Saint Elian score, Texas using the corresponding 4 × 4 table, and WIfI calculated by the mobile application SVS. The toe brachial index or transcutaneous oxygen pressure were not used to calculate WIfI score because of the lack of that technology. Patients were treated at a tertiary care hospital by a multidisciplinary team that includes a vascular surgeon, a clinician diabetologist physician, an orthopedist surgeon, a physiatrist, an infectologist, podiatrist, and nurse. Patients were treated ambulatory or hospitalized depending on the severity of the wound according to the recommendations of international guidelines for diabetic foot management from different societies (IDSA guidelines 10, D-foot international 11 and NICE guidelines 12). If the wound was clinically infected, microbiological cultures were taken and empirical antibiotic therapy was initiated guided by local germs. If the patient had severe ischemia, the medical team ordered angiography and revascularization that was carried out in the same hospital.
Decisions on major or minor amputation were taken by the team guided by international guidelines and clinical judgement.
Large ischemic ulcers without possibility of revascularization, life threatening lesions or sepsis were some indications for major amputation. Wound cleansing was carried out using physiological solution or water for non-infected wounds and chlorhexidine 4% if they were to require antisepsis. If the patient had severe ischemia, the medical team ordered angiography and revascularization that was carried out in the same hospital. Surgical or chemical debridement was performed as needed, and collagenase, hydrogel, and alginate were used.
Wound dressings were used when available. This study was approved by Investigation and Research department and Ethics Committee. Informed consent was not necessary, but a written notice that clinical trial was being performed was shown to the patients. Data and information were used and analyzed in an anonymous fashion. This is a descriptive study and investigation was carried out protecting identity of patients.
Categorical variables are presented as absolute values and percentage. Continuous variables are presented as mean and standard deviation or median and IQ range. For comparison between categorical variables, χ2 was used, and for continuous variables, median comparisons were performed with Student’s test for normal distribution and Mann-Whitney test for asymmetrical distribution. Kruskal-Wallis test was used to determine if there were differences between 2 or more groups of an independent variable on a continuous or ordinal dependent variable. Infostat, MedCalc, SPSS, and VCCstat were used for the statistical analysis. Significance was considered as < 0.05. Values for χ2 with Yates correction or the Fisher’s exact test with 2 × 2 tables and of variance ratios for natural and treatment analysis of variance were calculated.
Results
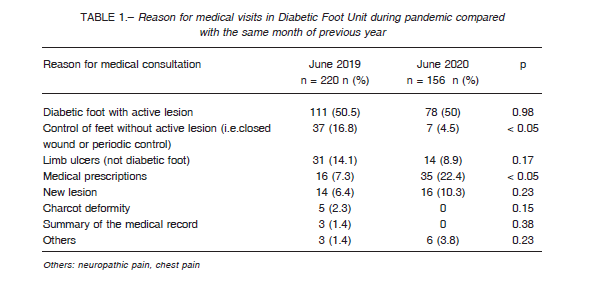
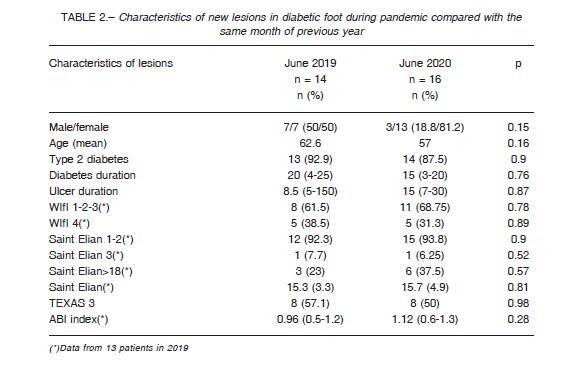
Data from 376 medical visits were analyzed; 220 were from June 2019 (retrospective analysis from database and medical records) and 156 from June 2020 (data prospectively collected). Characteristics of medical visits during each year are shown in Table 1. Fourteen patients consulted with new lesions during June 2019. Three could not identify the cause of the lesion (21.4%), while plantar pressures in neuropathic foot, trauma and friction against the shoe were recognized as the cause of the diabetic foot in 2, each with 14.3%. Sixteen patients consulted in 2020 because of new lesions. Most of them (43.7%) did not recognize the cause of the lesions, while 3 (18.8%) were due to plantar pressure in a neuropathic foot, 2 (12.5%) secondary to trauma and friction against the shoe and 2 (12.5%) because of other causes (p = ns). More information about new lesions is shown in Table 2. In all patients that consulted with new lesions during both years (n = 30), data on ABI index was obtained in 29. From them, 11 (37.9%) had an ABI less than 0.9, which implies some kind of peripheral arterial disease. This proportion was 46.2% (n = 6) in 2019 and 31.3% (n = 5) in 2020 (p = 0.66). In 2019, there were 3 visits (1.4%) in which relatives or carers did the consultation, just to get prescriptions or to ask for medical summaries instead of patients. This kind of consultation increased in 2020 to 25 visits (16.3%) (p < 0.01).
During 2019, telehealth consults were not recorded, and in 2020 there were 11 medical consultation registered in this modality, representing a 7% of all medical visits. There were no major amputations during June 2019 and there were 4 major amputations during June 2020. In the course of June 2020, 3 patients manifested COVID-19 symptoms during diabetic foot visit and had to undergo a COVID-19 test. One of them had a positive test.
Discussion
COVID-19 outbreak was an unexpected disease that constituted the beginning of a new reality, disrupting all aspects of clinical practice. Physicians had to design new strategies for treating and managing other diseases, trying to keep patients with diabetic foot disease free from the hospital without leaving them unattended. Most literature on diabetic foot and COVID-19 are recommendations and guidelines. In a study accepted for publication13 in the UK, routinely collected data on new diabetic foot ulcers from medical reports were retrospectively analyzed, finding a 52% reduction in the incidence of new ulcers during pandemic. In our study, we found a 29% reduction in diabetic foot visits, but a slight augment in the consultation for new lesions. Another finding was that more consults were performed by telehealth or through relatives’ visits in our hospital. Before pandemic, carers usually attended the consultation instead of the patients so as to obtain a medical prescription when, for some reasons, patients could not attend medical appointments themselves. During pandemic, carers and relatives did not want the patients to go to the hospital unless a severe foot lesion had developed, because of the risk conferred by diabetes to patients during COVID-19. This was shown in our study, where we found that number of visits from patients’ relatives was higher during June 2020 than during June 2019 (16.3% to 1.4%) (p < 0.01).We could see how telehealth consults rose as a tool for control of stable lesions, representing an 11% of all visits in 2020 (although we could not make a comparison to 2019 because of the absence of previous records), and how relatives had to get involved in the patient’s care, helping to avoid the visit to the hospital of high-risk diabetic people. In the case of telehealth, many clinicians around the world have shifted to this modality 14. The most frequently method used in diabetic foot consultation was photos with instant messaging, as these are accessible to patients or their carers, and that is the way our foot unit is managing at present when performing a telehealth consult. But diagnosing based on a photo is not always very reliable, and even triaging for treatment urgency differs between clinicians 14. Patients must understand that this type of medical consultation is an exception because of the pandemic and medical visits must be resumed when this situation ends. Physicians should be aware that patients with limb-or life-threatening problems should always be seen urgently. Those with new lesions lasted 8.5 days from lesion development until consultation in 2019 and 15 in 2020, but this difference was not statistically significant (p = ns). Conditions to be treated in hospital are diabetic foot attack 5, critical ischemia, infection that does not improve with home treatment.
Conditions to be treated at home include mild infections, not infected and non ischemic ulcers, acute Charcot. Other concerns include that diabetic foot is a leading cause of bed occupation and during COVID-19 health systems need more physical resources to manage COVID, with less physical resources then available to manage diabetic foot infections 15. Efforts must be focused on avoiding hospitalization when possible, by performing immediate surgical drainages and giving antibiotic treatment in an ambulatory setting or by shortening hospitalization as much as possible. In spite of these strategies, several patients presented with severe lesions that require hospitalization.
In the last month, three that consulted because of a diabetic foot had symptoms of coronavirus and one of them was positive for COVID-19. This fact warns physicians to take precautions when they treat diabetic foot patients using personal protection equipment and pay attention to respiratory symptoms. When data collection for this study ended, there were more than 60 000 positive cases and 1200 deaths and 50% of bed occupation, starting a more severe phase of social isolating. A new period of uncertainty about the outcomes of diabetic foot patients is starting in our country, with some studies predicting a long period of confinement 16. Limitations of this study include different factors as the short span of time data has been collected and the different behaviors of medical visits depending the moment of the quarantine, thus making this information a photograph of one moment that constantly changes.
More studies about this topic are necessary to analize the behavior of this pathology in relation to the pandemic, with the aim of making accurate decisions based on evidence.
Acknowledgements: To Ethical Committee for the guidance to perform the study and Dr. Matías Baldini for helping in the writing. To Mrs. Julieta Pagani and Mrs. Rosalía Urbano for the translation.
Conflict of interest: None to declare
References
1. WHO Director-General´s opening remarks at the media briefing of COVID-19 – 27 February 2020. In: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-27-february-2020; accessed March 2020.
2. Watkins J. Preventing a COVID-19 pandemic. BMJ 2020; 368:m810.
3. Nuevo Coronavirus 2019. Información, recomendaciones del Ministerio de Salud de la Nación y medidas de prevención. In: https://www.argentina.gob.ar/salud/coronavirus-COVID-19; accessed May 2020.
4. Armstrong D, Boulton A, Bus S. Diabetic foot ulcers and their recurrence. N Engl J Med 2017; 376: 2367-75.
5. Vas P, Edmonds M, Kavarthapu V, et al. The Diabetic Foot Attack: “’Tis Too Late to Retreat!” Int J Low Extrem Wounds 2018; 17: 7-13
6. Papanas N, Papachristou S. Covid-19 and diabetic foot: will the lamp burn bright? Int J Low Extrem Wounds 2020; 19: 111.
7. Martinez de Jesús FA. Checklist system to score healing progress of diabetic foot ulcers. Int J Low Extrem Wounds 2010; 9: 74-83.
8. Mathioudakis N, Hicks C, Canner J, et al. The society for vascular surgery wound, ischemia, and foot infection (WIfI) classification system predicts wound healing but not major amputation in patients with diabetic foot ulcers treated in a multidisciplinary setting. J Vasc Surg 2017; 65: 1698-705.
9. Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998; 21: 855-59.
10. Lipsky B, Berendt A, Cornia P, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infection. Clin Infect Dis 2012; 54:1679-84.
11. D-Foot International. The International Working Group on the Diabetic Foot Guidance (IWGDF Guidance) produces international, multidisciplinary, evidence-based guidance documents on diabetic foot. Updated 2019. In: https://dfoot.org/resources/resources/iwgdf-guidancedocuments ; accessed May 2020
12. National Institute for Health and Care Excellence. Diabetic foot problems: prevention and management. NICE guidelines [N19]. Published August 26, 2015. Updated October 11, 2019. In: https://www.nice.org.uk/guidance/ng19; accessed May 2020
13. Lipscomb D, Smith AS, Adamson S, Rezazadeh EM. Diabetic foot ulceration in COVID-19 lockdown: cause for concern or unexpected benefit? Diabetic Medicine 2020 In: https://doi.org/10.1111/dme.14340 Peer reviewed and accepted; accessed June 2020.
14. Covid-19 and diabetic foot disease. IWGDF. In: https://iwgdfguidelines.org/ ; accessed June 2020.
15. Coronavirus. Managing diabetic foot disease in the COVID crisis. Diabetic foot Australia In: https://www.diabeticfootaustralia.org/; accessed June 2020
16. Borracci R, Giglio N. Estimación del efecto del distanciamiento social sobre la epidemia de COVID-19 de otoño-invierno en el área metropolitana de Buenos Aires. Medicina (B Aires) 2020; 80 (Supl. III): 7-15.
