VILMA A. TRIPODORO 1, 2, VICTORIA LLANOS 1, 2, SILVINA DE LELLIS 2, CECILIA SALAZAR GÜEMES 1, GABRIEL G. DE SIMONE 2, 3, XAVIER GÓMEZ-BATISTE 4, 5
1Instituto de Investigaciones Médicas Alfredo Lanari, Universidad de Buenos Aires, Argentina, 2Instituto Pallium Latinoamérica, Buenos Aires, Argentina, 3Hospital de Gastroenterología Carlos B. Udaondo, Buenos Aires, Argentina, 4Cátedra de Cuidados Paliativos, Universidad de Vic, Barcelona, España, 5The Qualy Observatory, WHO Collaborating Centre for Palliative Care Public Health Programs (WHOCC), Catalan Institute of Oncology, Barcelona, Spain
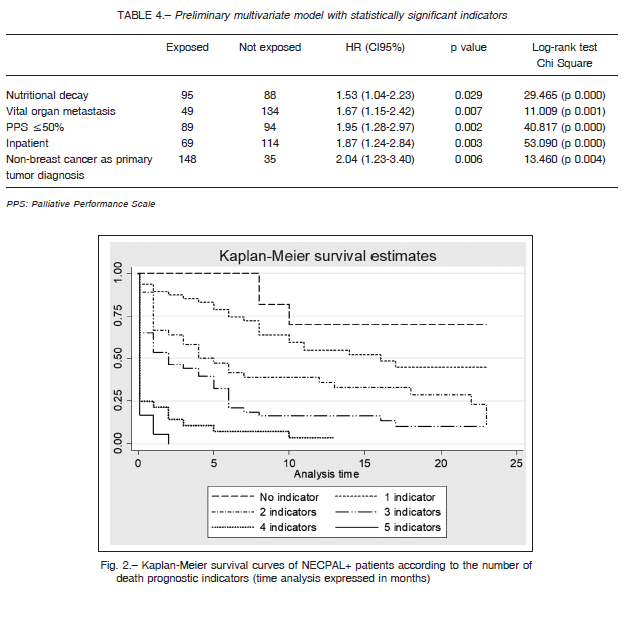
Abstract The early identification of patients with palliative needs has shown benefits in terms of quality of life and treatment goals. No prospective methods have been applied in Argentina to identify palliative needs in cancer patients. The NECPAL tool combines the physician’s own insight with objective indicators of disease progression and indicators of chronic advanced conditions. The aim of this study was to identify prognostic factors of mortality in hospitalized and ambulatory patients with cancer and palliative needs according to the NECPAL tool in a University Hospital in Buenos Aires city. Study variables were obtained by interviews with 10 physicians in charge of 317 patients with cancer over a 2-year follow-up period. A total of 183 patients with palliative needs were labelled as NECPAL+. Of these, 137 died after a median 4-month follow-up period. The death rate was 11% patients/month. The mortality was higher in inpatients during the first month (p < 0.003). In the multivariate model, the best predictors of mortality combining relevant indicators were: inpatients (HR 1.87; 95% CI 1.24-2.84; p = 0.003), initial diagnosis other than breast cancer (HR 2.04; 95% CI 1.23-3.40; p = 0.006), metastatic disease (HR 1.67; 95% CI 1.15-2.42; p = 0.007), functional deterioration (HR 1.95; 95% CI 1.28-2.97; p = 0.002), and malnutrition (HR 1.53; 95% CI 1.04-2.23; p = 0.029). The major breakthrough was the systematic prospective identification of palliative needs in cancer patients for the first time in Argentina. The NECPAL tool can improve the prediction of mortality in hospital settings.
Key words: advanced cancer, palliative care, chronic disease, prognosis, mortality
Resumen Factores pronósticos en pacientes con cáncer y necesidades paliativas identificados con el instrumento NECPAL CCOMS-ICO ©. La identificación temprana de pacientes con necesidades paliativas ha demostrado beneficios en términos de calidad de vida y objetivos de tratamiento. En Argentina no han sido aplicados métodos prospectivos para identificar necesidades paliativas en pacientes con cáncer. El NECPAL CCOMS-ICO © combina la percepción del médico con indicadores objetivos de progresión de enfermedades crónicas avanzadas y es útil para determinar la prevalencia de pacientes con necesidades paliativas en la población general. El objetivo fue identificar factores pronósticos de mortalidad en pacientes internados y ambulatorios con cáncer y necesidades paliativas según NECPAL en un Hospital Universitario de la ciudad de Buenos Aires. Las variables se obtuvieron mediante entrevistas a 10 médicos a cargo de 317 pacientes con cáncer y necesidades paliativas durante dos años de seguimiento. Los predictores de mortalidad en el modelo multivariado fueron: hospitalización (HR 1.87; IC 95% 1.24-2.84; p = 0.003), diagnóstico distinto de cáncer de mama (HR 2.04; IC 95% 1.23-3.40; p = 0.006), enfermedad metastásica (HR 1.67; IC 95% 1.15-2.42; p = 0.007), deterioro funcional (HR 1.95; IC 95% 1.28-2.97; p = 0.002) y nutricional (HR 1.53; IC 95% 1.04-2.23; p = 0.029). De los 183 pacientes con necesidades paliativas identificados como NECPAL+, 137 murieron en un período medio de 4 meses. La tasa de mortalidad fue 11% por mes. La mortalidad fue mayor (p < 0.003) en el primer mes de hospitalización. El mayor logro fue la identificación sistemática y prospectiva, por primera vez en Argentina, de necesidades paliativas en pacientes con cáncer. La herramienta NECPAL puede mejorar la predicción de la mortalidad en entornos hospitalarios.
Palabras clave: cáncer avanzado, cuidados paliativos, enfermedad crónica, pronóstico, mortalidad
Dirección postal: Vilma A. Tripodoro, Instituto de Investigaciones Médicas Alfredo Lanari, Universidad de Buenos Aires, Combatientes de Malvinas 3150, 1427 Buenos Aires, Argentina
e-mail: vilma.tripodoro@gmail.com
Palliative care (PC) has been successfully introduced into the public health system of many countries. The World Health Assembly (WHA) recommends strengthening PC as a part of a comprehensive healthcare approach that encourages all countries to design and implement PC programs in all levels of attention 1. Nevertheless, the development is unequal 1, 2.
The early identification and the multidimensional assessment of palliative needs have shown clear benefits in terms of symptom control, quality of life, and treatment goals 3-8. Patients who have access to specialized PC have better clinical outcomes with potentially lower treatment costs 3, 9, 10. They also receive less aggressive end of life care and survive longer 11, 12.
Using the NECPAL CCOMS-ICO© (hereafter NECPAL tool), which has been content-validated in the Catalonian public health system, the prevalence of patients with PC needs was estimated in 1.5% in the general population3. Growing evidence shows that the NECPAL tool is useful to detect individuals with advanced chronic diseases (ACD) and PC needs and that it can be used to determine the prevalence in specific healthcare settings and in the general population 3, 6, 8. The use of a combination of several parameters in the assessment increases its accuracy as a screening tool 13, 14. The validated NECPAL tool is freely available in Spanish, Catalan and English at http://ico.gencat.cat/en/professionals/serveis_i_programes/observatori_qualy/eines_de_suport/eines/instrument_i_programa/.
Argentina has a medium-high incidence of cancer with over 100 000 new cases per year, in both men and women, and ranks seventh in terms of incidence and third in terms of mortality among countries of the American region 15-17.
Understanding the need of PC is essential for healthcare service planning 3. The methods used to estimate PC need in the general population vary according to the different approaches and data sources. In 2016, the National Cancer Institute (Argentina) launched the National PC Program with emphasis on suffering prevention and the improvement of quality of life of cancer patients and their families 18. Nevertheless, it does not establish a method to identify early PC needs in the target population. In the first study carried out with the NECPAL tool in Buenos Aires city, we found that 1 every 3 patients with ACD (cancer or non-cancer) could die within one year and had a clear need for PC. There are no PC public health programs running in the city so far 19. Identifying patients with PC needs and accurately predicting mortality would facilitate a timely and efficient delivery of end of life care.
This study aims to identify prognostic factors of mortality in cancer patients with PC needs in our cultural context using for the first the NECPAL tool, a validated predictive instrument. It is part of the NECPAL Model Program carried out at the Instituto de Investigaciones Médicas Alfredo Lanari, Universidad de Buenos Aires, and Pallium Latinoamérica.
Materials and methods
A 2-year prospective follow-up study was carried out in 2014-2016. All consecutive inpatients and outpatients = 18 years old
with cancer registered in our hospital were included.
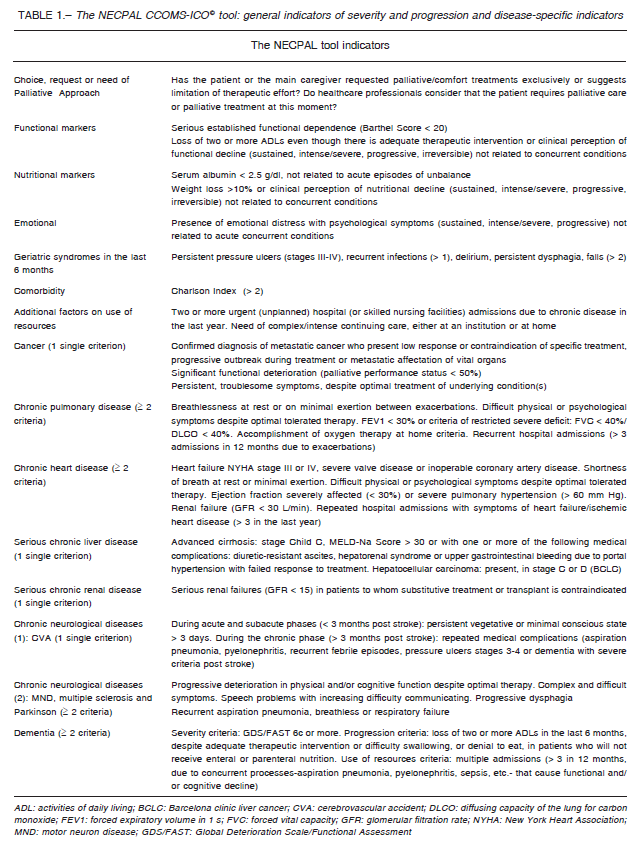
The data was gathered by interviews with the medical staff in charge according to the NECPAL tool Manual for Databases20. This tool provides both quantitative and qualitative evaluations. It offers a multifactorial, nondichotomous assessment process that combines subjective perception (the surprise question [SQ]: Would you be surprised if this patient dies in the next year?) with other parameters, including the request (and need) for PC, the assessment of disease severity and progression, geriatric syndromes, psychosocial factors, and comorbidities (Charlson comorbidity index), as well as the use of health resources. It also includes specific indicators for selected illnesses (Table 1) 20. Patients considered NECPAL positive (+) are SQ+ patients who also fulfill at least one of the other parameters of the tool.
Socio-demographic and medical data were collected from medical records. Variables assessed were age, sex, patient’s condition as inpatient or outpatient, diagnosis, nutritional status, performance status (Palliative Performance Scale), presence of metastases, specialty of the attending physician (oncologist, urologist, gynecologist, internist, oncohematologist, PC specialist) and date and time of the first visit to the PC ward.
The variables were obtained by interviews with the 10 physicians in charge (69 individual interviews) and by reviewing the clinical records. One evaluator conducted all staff interviews. The patients, identified only by their physicians, were stratified according to four levels of disease: Level 0 cancer (n:317); Level 1 cancer with ACD (n:226); Level 2 cancer with SQ+ (n:183); Level 3 NECPAL+ cancer with SQ+ and at least one indicator listed in Table 1 (n:183). All NECPAL+ patients were followed for 2 years since first detected as such.
Data were anonymized and collected in a digital database. A descriptive analysis was conducted on the demographic and clinical parameters of patients NECPAL+. Continuous variables were expressed as mean values ± standard deviation and median and range according to distribution.
Survival Kaplan-Meier curves were generated from the date of the patient’s identification as NECPAL+ to her/his date of death or last control (2 years). The Log Rank test was used to compare the different groups according to age, gender, primary diagnosis (breast cancer versus other tumors), and patient’s condition as inpatient or outpatient. Nutritional status and Palliative Performance Scale or the presence of vital organ metastases and hazard ratios were calculated with the Cox’s proportional hazard model. A multivariate model was built to explore the best predictors of mortality, using the variables that stood out as significant in the univariate analysis with the Cox’s proportional hazard model. A p < 0.05 value was considered significant. The study was approved by the Ethics Committees of the institutions involved in the NECPAL Program, Instituto A. Lanari and Instituto Pallium Latinoamérica.
The statistical analysis was carried out by the Statistical Package for Social Science (IBM-SPSS 22 version (SPSS Inc. Chicago, IL)) program and by Stata V12.
Results
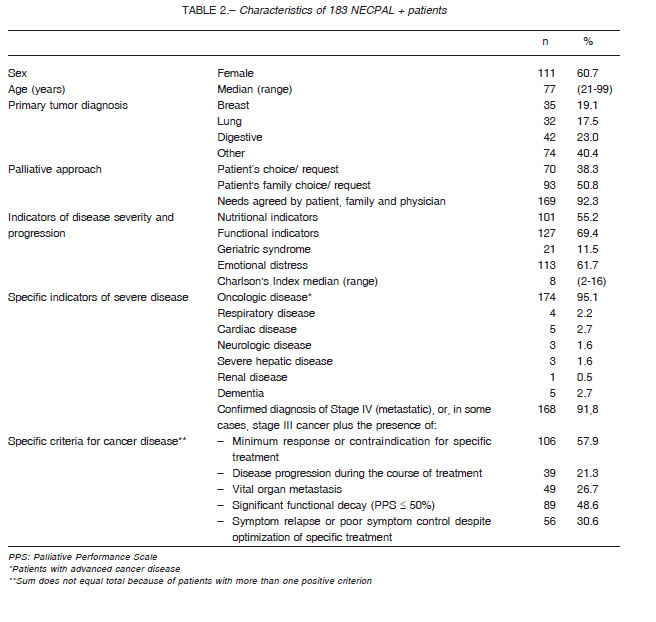
A total of 317 cancer patients were evaluated; 246 (77.6%) were ambulatory at the time of identification and 211 (66.6%) were women. The median age was 77 years (range 21-99). Table 2 describes the 183 patients identified as NECPAL+ (Level 3).
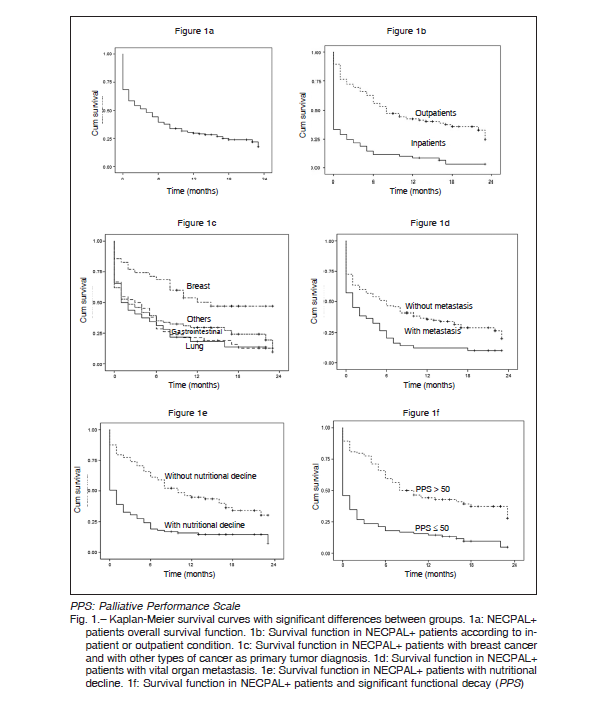
During the follow-up period, 137 NECPAL+ patients died. The median follow-up period was 4 months for the entire sample but for the 46 patients who did not die, the median follow-up period was 17 months (range 9-23). No patient reached a 24 month follow-up. Figure 1 shows survival curves for the 137 NECPAL+ dead patients: Figure 1a shows the cumulative survival of the entire study population. The overall death rate was 11% patients/month (median 4 months). No significant differences were
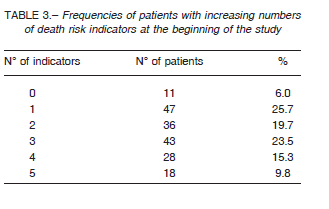
found in mortality between men and women or between the different age groups (< 75 vs. = 75 years old). In turn, a significantly higher mortality was found during the first month of follow-up for patients who were hospitalized at the moment of identification as NECPAL+ (Fig. 1b). Significant differences were also found when comparing breast vs. other cancers (Fig. 1c), presence vs. absence of metastasis in vital organ (Fig. 1d), presence vs. absence of nutritional decay (Fig. 1e), and Palliative Performance values > 50 vs. = 50 (Fig. 1f). Table 3 shows frequencies of patients with increasing numbers of death risk indicators at the beginning of follow-up.
A preliminary multivariate model was built using these significant variables in a binomial codification (individuals exposed and not exposed to these conditions) (Table 4). Figure 2 shows survival of NECPAL+ patients with different prognostic indicators. Patients who were hospitalized, whose primary cancer localization was other than breast, who had metastatic disease, functional decline (assessed with the Palliative Performance Scale), or nutritional decline showed a considerable lower survival rate.
Discussion
We present results of a systematic study on death prognosis factors of cancer patients with palliative needs carried out in Argentina. Both, prognosis and palliative needs, are central aspects of end of life care because they play a central role in care decision making in line with patients’ values, preferences and aims 14, 21. The major breakthrough was the successful use of a direct prospective method of systematic risk assessment in cancer patients with palliative care needs, aimed to improve the prediction of mortality in hospital settings. The consequences of not identifying these two aspects on time may lead to inadequate symptom control, inappropriate use of health resources and the absence of planning for decision making 3, 21.
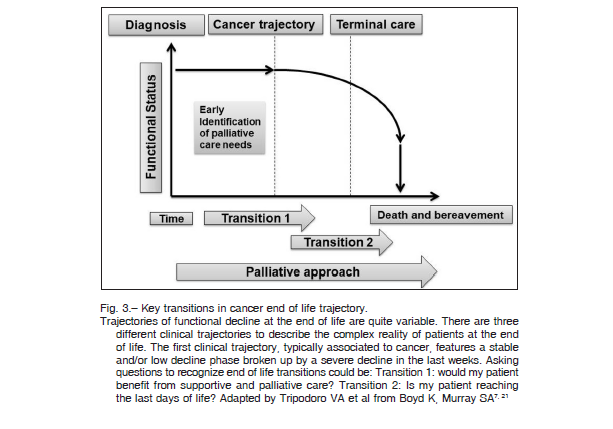
The NECPAL tool resulted useful in our university hospital setting for the identification of prognostic factors and mortality risk factors in coincidence with results published by Spanish authors 13, 14. It was useful to describe the survival rate after 12 and 24-month follow-up because the 12-month period is exactly the NECPAL tool’s point of interest, endorsing the conceptual approach of typical trajectories of decline in ACD (Fig. 3) 3, 8, 21, 22.
The presence of ACD has the largest impact on life expectancy and quality of life, especially in elderly people 23. The percentage of patients with PC needs or NECPAL+ in our study was 57.7%. Additionally, most of them had marked functional decline and malnutrition (Table 2). Similarly, in a university hospital in Catalonia nearly 40% of patients were NECPAL+ 24. In these patients, the benefits of cancer treatment are very limited due to a reduction of life expectancy and an increase of side-effects complications 25. The early identification of patients at high risk of death would allow the implementation of early intervention programs to improve PC 26. This is clearly the best choice for patients at high risk of treatment complications and for whom life expectancy without cancer is even shorter than life expectancy with cancer 25.
Even if nowadays cancer is no longer the deadly disease that it used to be, near one every three individuals in the western world will develop some sort of cancer at some point of his/her life 26. According to the WHO’s estimations, 80% of the population who died from malignant tumors could had required PC1. The cancer mortality rate in Argentina is 115.1/100 000 inhabitants; it means 50 000 people dying of cancer are in need of PC 16. Nevertheless, these estimates include only cancer-related mortality and consider only end of life conditions and therefore are underestimating the real need for PC by not including comorbidities 5, 16, 18, 19. Because of the prospective design of our study, we could establish the prevalence and timely clinical follow up of cancer patients with PC needs.
The NECPAL tool, including the SQ, was developed for use in a primary care setting 3, 22, 27-32. The SQ has also proved to be useful in the hospital setting 33. Furthermore, it is the only tool which takes into account the patient’s or his family’s expression of PC need, as well as the presence of severe social or emotional distress 28.
A total of 81% of our patients were found to have some sort of underlying ACD and 81% of these had a SQ+. The same patients had at least one additional criterion of disease severity and progression and therefore were considered NECPAL+. In general practice, the SQ predicted a 12-month survival time in cancer patients in stage IV with 69.3% sensitivity and 83.6% specificity 27, 28. In the current study, we did not analyze sensitivity and specificity with ROC curves; however, we found 100% correlation between level 2 (SQ+) and level 3 (SQ+ plus one indicator). The SQ has proved to be a predictor of mortality in specific diseases and settings, primarily cancer28. The NECPAL tool, which combines the SQ with additional indicators, can be used to screen patients for early palliative care with a reasonable degree of predictive accuracy. Nevertheless, the coincidence between level 2 and 3 in our setting opens a new research question. Is the SQ by itself, a good predictor of bad prognosis or, the cancer in our patients was not diagnosed timely enough and they were severely affected at first consultation or hospitalization? Additional research is needed to answer this question.
As seen in Table 2, elderly people were the most affected by functional decline, malnutrition, and comorbidity. Compared with the Charlson comorbidity index, the NECPAL tool is a better predictor of mortality at 6 and 24 months 33. In our study, almost half of NECPAL+ patients had a significant functional decline. In NECPAL+ patients, specific treatments have a poor response or are contraindicated. Our very high 2-year mortality (74.8%) with a very short median survival (4 months) shows the severity of the clinical conditions involved. Most probably, this is not only reflecting the primary cancer condition but also old age and comorbidities (Table 2) in inpatients.
We constructed a predictive model to identify individuals with PC needs for a 24-month period using the multivariate analysis of a combination of relevant indicators, i.e. hospitalization, cancer other than breast as primary diagnosis, metastases, functional decline, and malnutrition. The concurrence of all such indicators correlated strongly with high mortality risk during the first month of follow-up. Regarding NECPAL tool capacity to predict mortality in cancer patients at 12 months, previous reports showed excellent discrimination ability and very good sensitivity and specificity, although this is not the aim of the tool 14, 28, 33.
We should emphasize that our study excluded all cancer patients who did not fulfill the SQ+ criterium. Thus, we were not able to compare mortality risk of SQ+ vs. SQ- patients. However, significant differences in 24-month mortality were indeed observed at among NECPAL+ and NECPAL- patients in a previous study performed in Catalonia 28.
The fact that half of the patients in our population died within 4 months suggests that they might had not been detected promptly enough. Some of the patients NECPAL+ in our study had been diagnosed in advanced stages of disease, therefore they obtained no benefit from specific treatment or had no chance to cure. In these cases, the only effective management is high quality PC to improve the quality of their end of life 21.
In our study, according to NECPAL tool criteria, healthcare professionals considered that 38% of the patients had palliative needs and half of their families requested PC either in an implicit or an explicit manner (Table 2).
The perception of malnutrition was more common in cancer patients (55.2%) than generally perceived in other ACD groups. The impact of nutritional decline as an important end of life marker in cancer patients is also consistent with what is seen in medical literature 13, 32-36. Individuals identified by our healthcare professionals as in need of PC had a risk of mortality > 3 times higher than those who were not 13. Both this relevant relationship and the fact that the best discrimination ability of the model is seen over 12 months, prove the predictability of the monophasic decline pattern typically seen in cancer patients 13.
End of life care comprises three overlapping phases of disease: from diagnosis to the beginning of supportive care, from this point to the beginning of end of life care, and end of life care until death (Fig. 3) 9, 21. During this progression, there are two turning points known as the first and the second transition. These are key moments in which palliative measures can be incorporated to the care plan to avoid disproportionate treatments and reduce unnecessary costs 9-11, 33, 36-39. According to their median survival, most of our patients were in the second transition, that is, closer to the end of their life (Fig. 3) 19, 21.
In the current study, the criteria for advanced cancer disease were functional decline and contraindication for specific treatment or minimum response to it. The distribution of primary tumor sites in our sample was in line with official statistics at the national level: breast, lung and colorectal localization 16. The presence of metastases in vital organs was infrequent, ~27%. Even bone metastases did not exceed 35%. High short-term mortality was probably caused by comorbidities and frailty syndrome (70% had functional decline).
A potential limitation of this study is that inclusion criteria are based on the subjective clinical judgment of healthcare professionals with different medical specialties. To reduce this bias, all definitions, procedures, and actions were standardized according to the procedure manual of the NECPAL CCOMS-ICO© tool 20. Our model for prognostic factors and mortality risk is probably applicable only to our population and its particular characteristics. However, we had already described in a previous study, that two out of three cancer patients affected by advanced disease could die in the next year and had palliative care needs 19.
In conclusion, the NECPAL tool is a valuable instrument that helps physicians to detect cancer patients with palliative needs and bad prognosis. What is more, the SQ+ can be considered a simple tool to determine when it is good to incorporate PC to patient management21. The NECPAL tool considers assessment of other variables like hospitalization, malignancy other than breast cancer, metastatic disease, functional decline, and malnutrition, all of which reinforce its value in the assessment of prognosis and mortality risk.
Acknowledgements: The authors thank Dr. M. Khoury, Dr. E. L. De Vito and Dr. T. Pastrana for their support and valuable suggestions. Pallium Latinoamérica and the National Cancer Institute funded the NECPAL Model Program.
Conflicts of interest: None to declare
References
1. World Health Assembly. Resolution WHA A67.19. Strengthening of palliative care as a component of comprehensive care throughout the life course. In: http://apps.who.int/ medicinedocs/en/d/Js21454en/; accessed September 2018.
2. Gómez-Batiste X, Martínez-Muñoz M, Blay C, Amblàs J, Vila L, Costa X. Identificación de personas con enfermedades crónicas avanzadas y necesidad de atención paliativa: elaboración del Instrumento NECPAL CCOMSICO© Med Clin (Barc) 2013; 140: 241-5.
3. Gómez Batiste X, Martínez Muñoz M, Blay C, et al. Prevalence and characteristics of patients with advanced chronic conditions in need of palliative care in the general population: A cross-sectional study. Palliat Med 2014; 28: 302-11.
4. Murtagh FE, Bausewein C, Verne J, Groeneveld EI, Kaloki YE, Higginson IJ. How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med 2014; 28: 49-58.
5. Higginson IJ. Health care needs assessment: palliative and terminal care. In: Stevens A, Raftery J (eds): Health care needs assessment. Oxford: Radcliffe Medical Press, 1997; p 1-28.
6. Gómez-Batiste X, Martínez-Muñoz M, Blay C, Espinosa J, Contel JC, Ledesma A. Identifying needs and improving palliative care of chronically ill patients: a community-oriented, population-based, public-health approach. Curr Opin Support Palliat Care 2012; 6: 371-8.
7. Tripodoro VA, De Vito EL. What does end stage in neuromuscular diseases mean? Key approach-based transitions. Curr Opin Support Palliat Care 2015; 9: 361-8.
8. Gómez Batiste X, Blay C, Roca J, Fontanals de Nadal M, Calsina-Berna A. Manual de atención integral de personas con enfermedades crónicas avanzadas. Aspectos generales. Principios generales de la atención paliativa. Barcelona: Elsevier 2014, p 51-5.
9. Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ 2005; 330: 1007-11.
10. Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 2008; 168: 1783-90.
11. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010; 363: 733-42.
12. Tripodoro V. Cómo identificar al paciente con necesidad de atención paliativa. In: Jacob G. Manual de Cuidados Paliativos para la Atención Primaria de Salud (1ra. ed). Argentina: Instituto Nacional del Cáncer, 2014, p 39-55.
13. Amblàs-Novellas J, Murray SA, Espaulella J, et al. Identifying patients with advanced chronic conditions for a progressive palliative care approach: a cross-sectional study of prognostic indicators related to end-of-life trajectories.
2016 BMJ Open In: https://bmjopen.bmj.com/content/6/9/e012340; accessed September 2018.
14. Martinez-Muñoz M. Identifying individuals with advanced chronic conditions who may benefit from an early palliative care approach: Using the NECPAL CCOMS-ICO© tool: population-based prevalence, predictive validity for mortality and predictive models. (Tesis doctoral). Universidad de VIC-Universidad Central de Cataluña 2016. In: http://repositori.uvic.cat/handle/10854/4814; accessed September 2018.
15. Ministerio de Salud de la Nación. Indicadores básicos. 2016. In: http://www.deis.msal.gov.ar/wpcontent/uploads/2018/04/IndicadoresBasicos2016.pdf; accessed September 2018.
16. Ministerio de Salud de la Nación. Sala de Situación del Cáncer en la República Argentina 2016. In: http://www. deis.msal.gov.ar/wp-content/uploads/2018/04/IndicadoresBasicos2016.pdf; accessed September 2018.
17. Bray F, Colombet M, Mery L, et al. Cancer Incidence in Five Continents, Vol. XI (electronic version). Lyon: International Agency for Research on Cancer. In: http://ci5. iarc.fr; accessed September 2018.
18. Boletín oficial del Ministerio de Salud de la Nación. Programa de Cuidados Paliativos. In: https://www.boletinoficial.gob.ar/#!DetalleNorma/150263/20160902; accessed September 2018.
19. Tripodoro V, Rynkiewicz C, Llanos V, Padova, De Lellis S, De Simone GG. Atención a personas con enfermedades crónicas avanzadas. Medicina (B Aires) 2016; 76: 139-47.
20. Gómez Batiste X, Martínez-Muñoz M, Blay C, et al. Instrumento NECPAL CCOMS-ICO© Manual para Base de datos. Observatorio “QUALY” – Centro Colaborador de la OMS para Programas Públicos de Cuidados Paliativos. Institut Català d’Oncologia. 2011. In: http://ico.gencat.cat/web/.content/minisite/ico/professionals/documents/qualy/arxius/doc_necpal_ccomsico_instrumento_esp_vweb_ vff.pdf; accessed September 2018.
21. Boyd K, Murray SA. Recognizing and managing key transitions in end of life care. BMJ 2010; 341: c4863.
22. Maas EA, Murray SA, Engels Y, Campbell C. What tools are available to identify patients with palliative care needs in primary care: a systematic literature review and survey of European practice. BMJ Support Palliat Care 2013; 3:
444-51.
23. Bengoa Rentería R. El reto de la cronicidad en España: mejor transformar que racionar. Gac Sanit 2015; 29: 323-5.
24. Gómez-Batiste X, Blay C, Martínez-Muñoz M, et al. The Catalonia WHO Demonstration Project of Palliative Care: Results at 25 years (1990-2015). J Pain Symptom Manage 2016; 52: 92-9.
25. Brighi N, Balducci L, Biasco G. Cancer in the elderly: Is it time for palliative care in geriatric oncology? J Geriatr Oncol 2014; 5: 197-203.
26. Tripodoro VA. El derecho a los cuidados paliativos o “el día en que la muerte decidió volver…” Medicina (B Aires)
2013; 73: 601-4.
27. Moroni M, Zocchi D, Bolognesi D, et al. The ‘surprise’ question in advanced cancer patients: A prospective study among general practitioners. Palliat Med 2014; 28: 959-64.
28. Gómez Batiste X, Martínez Muñoz M, Blay C, et al. Utility of the NECPAL CCOMS-ICO© tool and the Surprise Question as screening tools for early palliative care and to predict mortality in patients with advanced chronic conditions: A cohort study. Palliat Med 2017; 31: 754-63.
29. The GSF Prognostic Indicator Guidance. 2011. In: http:// www.goldstandardsframework.org.uk/evidence; accessed September 2018.
30. Highet G, Crawford D, Murray SA, Boyd K. Development and evaluation of the Supportive and Palliative Care Indicators Tool (SPICT): a mixed-methods study. BMJ Support Palliat Care 2014; 4: 285-90.
31. Thoonsen B, Engels Y, van Rijswijk E, et al. Early identification of palliative care patients in general practice: development of RADboud indicators for Palliative Care Needs (RADPAC). Br J Gen Pract 2012; 62: 625-31.
32. Moss AH, Lunney JR, Culp S, et al. Prognostic significance of the ‘Surprise’ question in cancer patients. J Palliat Med
2010; 13: 837-40.
33. Calsina-Berna A, Martinez-Muñoz M, Bardés Robles I, Beas Alba E, Madariaga Sánchez R, Gómez Batiste Alentorn X. Intrahospital mortality and survival of patients with advanced chronic illnesses in a tertiary hospital identified with the NECPAL CCOMS-ICOa tool. J Palliat Med 2018 21: 665-73.
34. Wie GA, Cho YA, Kim SY, Kim SM, Bae JM, Joung H. Prevalence and risk factors of malnutrition among cancer patients according to tumor location and stage in The National Cancer Center in Korea. Nutrition 2010; 26: 263-8.
35. Pressoir M, Desné S, Berchery D, et al. Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer 2010; 102: 966-71.
36. Aaldriks AA, van der Geest LGM, Giltay EJ, et al. Frailty and malnutrition predictive of mortality risk in older patients with advanced colorectal cancer receiving chemotherapy. J Geriatr Oncol 2013; 4: 218-26.
37. Parikh RB, Kirch RA, Smith TJ, Parikh RB, Temel JS. Early specialty palliative care-translating data in oncology into practice. N Engl J Med 2013; 369: 2347-51.
38. Howie L, Peppercorn J. Early palliative care in cancer treatment: rationale, evidence and clinical implications. Ther Adv Med Oncol 2013; 5: 318-23.
39. Blay C, Limón E, Meléndez A. Cronicidad, profesionalismo y la encrucijada paliativa. Medicina Paliativa 2017; 24: 1-3.
