RAUL A. BORRACCI1, 2, CARLOS A. INGINO2, JULIO MACIAS MIRANDA2
1Departamento de Cirugía Cardíaca, Hospital de Clínicas, Facultad de Medicina, Universidad de Buenos Aires, 2Departamento de Cardiología y Cirugía Cardíaca, ENERI-Sagrada Familia, Buenos Aires, Argentina
Abstract
The relationship between higher body mass index (BMI), decreased morbidity and mortality is known as the “obesity paradox”, and has been described in cohorts of patients with hypertension, diabetes, heart failure, coronary and peripheral artery diseases, non-cardiac surgery, and end-stage renal disease. Here we investigated the relationship between BMI and short-term outcomes after adult cardiac surgery to explore the existence of an obesity paradoxical effect. A secondary objective was to perform an updated systematic review to further analyze the association between BMI and 30-day in-hospital mortality after cardiac surgery. A retrospective analysis was performed from a consecutive series of 1823 adult patients who underwent cardiac surgery, that were assigned to five BMI groups: normal weight (18.5-24.9 kg/m²), overweight (25-29.9 kg/m²), class I obese (30-34.9 kg/m²), class II obese (35-39.9 kg/m²), and class III obese or morbidly obese (40-49.9 kg/m²). A systematic review search was performed including controlled trials and observational studies identified in MEDLINE, Embase, SCOPUS, and the Cochrane library (to the end of June 2017). In the present series, overweight and obese patients had similar or slightly lower in-hospital mortality rates after cardiac surgery compared with normal-weight individuals. Conversely, postoperative complication rates increased with higher BMI levels. Most studies included in the review showed that overweight and obese patients had at least the same mortality rate as normal-weight patients, or even a lower death risk. Pooled-data of the meta-analysis provided evidence on the association between higher BMI levels and a lower all-cause in-hospital mortality rate after cardiac surgery.
Key words: obesity, operative risk, cardiac surgery, meta-analysis
Resumen
Asociación entre índice de masa corporal y resultados a corto plazo después de la cirugía cardíaca: estudio retrospectivo y metaanálisis. La relación entre mayor índice de masa corporal (IMC) y menor morbilidad y mortalidad se conoce como “paradoja de la obesidad”. Se ha descrito en cohortes de pacientes con hipertensión, diabetes, insuficiencia cardíaca, enfermedad coronaria y arterial periférica, cirugías no cardíacas y enfermedad renal en etapa terminal. Aquí se investigó la relación entre IMC y resultados a corto plazo después de cirugía cardíaca en adultos, y la manifestación de la paradoja de la obesidad. También se realizó una revisión sistemática sobre asociación entre IMC y mortalidad a 30 días de la cirugía cardíaca. Se hizo un análisis retrospectivo de una serie consecutiva de 1823 adultos con cirugía cardíaca, asignados a cinco grupos de IMC: peso normal (18.5-24.9 kg/m²), sobrepeso (25- 29.9 kg/m²), obesidad clase I (30-34.9 kg/m²), clase II (35-39.9 kg/m²), y clase III (40-49.9 kg/m²), y una búsqueda sistemática de ensayos controlados y estudios observacionales en MEDLINE, Embase, SCOPUS y Cochrane (hasta 30/6/2017). En la serie, las tasas de mortalidad hospitalaria fueron similares o ligeramente menores en pacientes con sobrepeso y obesidad comparados con aquellos de peso normal. Pero también las tasas de complicaciones postoperatorias aumentaron con el IMC. La mayoría de los estudios observacionales revisados mostraron que los pacientes con sobrepeso y obesidad tenían al menos similar tasa de mortalidad que aquellos con peso normal, o menor riesgo de muerte. Los datos combinados del metaanálisis evidenciaron asociación entre los niveles de IMC mayores y tasa de mortalidad hospitalaria más baja después de cirugía cardíaca.
Palabras clave: obesidad, riesgo operatorio, cirugía cardíaca, metaanálisis
Recibido: 8-I-2018 Aceptado: 30-V-2018
Dirección postal: Dr. Raúl A. Borracci, La Pampa 3030, 1428 Buenos Aires, Argentina
e-mail: raborracci@gmail.com
Obesity has been described as a risk factor for the development of coronary artery disease, stroke, cancer, renovascular disease, and other physical and psychological comorbidities1-5. Conversely, several other epidemiological and observational studies on different diseases have shown better outcomes and survival rates in overweight and obese patients than in those with normal body mass index (BMI)6. This counter-intuitive relationship between higher BMI and decreased morbidity and mortality is known as the “obesity paradox”7, and has been observed in patients with hypertension, diabetes, heart failure, coronary and peripheral artery diseases, non-cardiac surgery, and end-stage renal disease8-10. However, studies examining the association between obesity and adverse outcomes after cardiac surgery still remain controversial11-15. For instance, the EuroSCORE II model does not include BMI as a predictive variable for stratification of perioperative death risk16. Some studies have demonstrated that overweight and moderately obese patients have better early hospital outcomes in terms of mortality11, 12, 17, and a lower incidence of major adverse cardiac and cerebrovascular events12, 17, 18. Other studies have not found any clear protective effect of overweight and obesity on mortality or adverse events after cardiac surgery19-21; or they have even demonstrated a deleterious effect for sternal wound infection22-25, leg infection26, sternal dehiscence27, renal failure23, 28, atrial fibrillation26, 29, venous thromboembolism29, and pulmonary and gastrointestinal complications30. In general, studies with negative evidence for the “obesity paradox” have tended to include far fewer patients than reports with positive evidence, a difference possibly related to the power analysis of sample size. Nevertheless, outcomes from large samples may in turn exaggerate the clinical value of a statistical difference.
The aim of this study was to investigate the relationship between BMI and short-term outcomes after adult cardiac surgery and to explore the existence of an obesity paradoxical effect. A secondary objective was to perform an updated systematic review to further analyze the association between BMI and 30-day in-hospital mortality after cardiac surgery.
Materials and methods
A retrospective analysis was performed on prospectively collected data (ambispective design) from a consecutive series of 1823 adult patients who underwent different types of cardiac surgery at the Buenos Aires University Hospital and its associated clinics over a 6-year period (2011-2016). All types of on-pump and off-pump elective cardiac surgery were included, except transplantation and transcatheter aortic valve implantation. Baseline and operative data were prospectively collected in a clinical registry, which included the variables needed to estimate the operative risk mortality based on EuroSCORE II16. Additional information on other risk factors and comorbidities was added in the computerized database. In-hospital major postoperative complications (stroke, cardiac arrest, myocardial infarction, renal dialysis, permanent pacemaker implantation, ventricular arrhythmias, reoperation for bleeding, low cardiac output, sternal dehiscence, deep sternal wound infection or mediastinitis, sepsis, prolonged ventilation, and pneumonia), and in-hospital mortality were compared among various BMI groups after cardiac surgery. BMI was automatically recorded in the operation theatre before surgery. Postoperatively, patients were assigned to five BMI groups31: normal weight (18.5 to 24.9 kg/m.), overweight (25 to 29.9 kg/m.), class I obese (30 to 34.9 kg/m.), class II obese (35 to 39.9 kg/m.), and class III obese or morbidly obese (40 to 49.9 kg/m.). Underweight (BMI < 18.5 kg/m.) (n = 3) and class IV or “super obese” (BMI ≥ 50 kg/m.) (n = 1) groups were excluded from the study due to the low number of patients.
Baseline preoperative clinical variables and in-hospital outcome data were recorded and analyzed with the approval of the local Institutional Review Board which waived the need for a written informed consent.
The systematic review search strategy was performed using controlled trials and observational studies identified in MEDLINE, Embase, SCOPUS, and the Cochrane library (to the end of June 2017). Reference lists of primary studies, review articles, and previous meta-analyses were reviewed with no language, age or type of cardiac surgery restrictions. The inclusion criteria required studies to separately report mortality in normal, overweight and obese patients using traditional World Health Organization BMI categories. Studies comparing obese versus non-obese patients (i.e. normal and overweight patients grouped together), and studies published only in abstract form were excluded from the analysis. Articles were also excluded if the total number of deaths was < 3. Two reviewers (R.A.B. and C.A.I.) independently reviewed citations and performed data retrieval, and disagreements were resolved through consensus. No additional data were requested from the primary study authors. The primary endpoint was all-cause mortality. Odds ratios (OR) with 95% confidence intervals (95% CI) and forest plots were calculated with EPIDAT, Version 3.1 (Xunta de Galicia-PAHO/WHO) using fixed and random effect models. Heterogeneity among studies was examined using the c. test and the Higgins I. test (25%, 50%, and 75% I. values were interpreted as low, moderate, and high heterogeneity). A funnel plot was used as a graphical method to identify studies affecting heterogeneity, and the Begg test to assess publication bias.
Categorical data were expressed as absolute frequencies and percentages, and continuous variables as mean and standard deviation (SD). The Kolmogorov-Smirnov (K-S) goodness-of-fit test was used to analyze normal distributions. Univariate comparison of discrete variables was performed using c. or Yates’ corrected c. test. Analysis for linear trends in proportions for postoperative complications was done with c. test for trend. One-way analysis of variance (ANOVA) was used to compare more than two means and post hoc multiple comparisons were done with Tukey’s test assuming equal variances. The Snedecor F-test was used to assess variance equality. Observed-to-expected operative mortality ratios within groups was also calculated and compared with the c. test. A propensity-score analysis was used to adjust for preoperative and operative confounding factors in order to minimize baseline differences between the BMI groups. Characteristics independently associated with normal and overweight or obese patients after propensity-score matching were assessed in a multivariate binary logistic regression model with backward stepwise conditional method. Covariates used in the regression model included all the preoperative and operative variables, and final results were expressed as odds ratio (OR) with the associated 95% CI. Non-linear regression analysis and the corresponding coefficient of determination (R.) were used to find the best fit for postoperative complications and mortality rates between BMI groups. Statistical analysis was performed with IBM SPSS 23.0 Statistics (IBM Corporation, Armonk, NY). A 2-tailed p value ≤ 0.05 was considered statistically significant.
Results
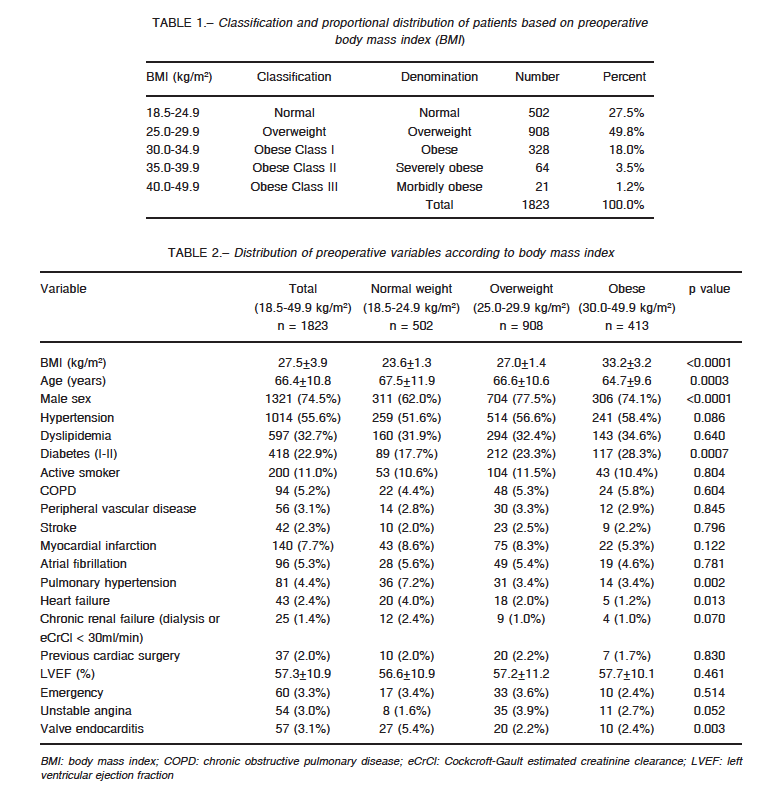
Classification and proportional distribution of patients based on preoperative BMI is shown in Table 1, where 22.7% (n = 413) was classified as obese, independently of class. For purpose analysis, all types of obesity were considered as a single group (aggregated BMI 30.0-49.9 kg/m.). Table 2 lists preoperative baseline characteristics of the BMI groups. Univariate analysis revealed younger age and higher rates of male sex and diabetes in overweight and obese patients compared with normal-weight individuals. Conversely, the normal-weight group showed higher rates of heart failure, pulmonary hypertension and heart valve endocarditis.
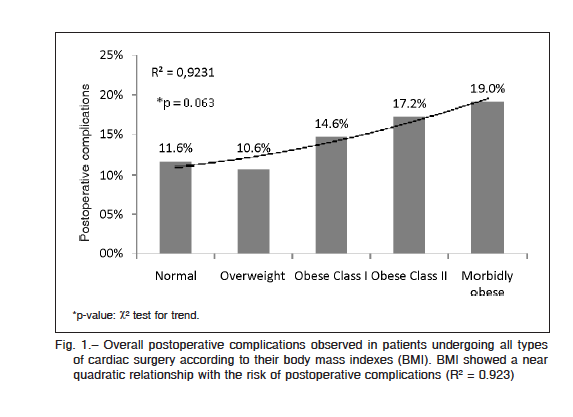
Distribution of operative variables and outcomes are shown in Table 3. Isolated coronary surgery and shorter cross-clamping time were more frequent in overweight and obese patients. Overall postoperative complications increased through BMI groups with a slight decrease in overweight patients (Table 3, Fig. 1). Postoperative ventricular arrhythmias were significantly more common in obese patients when complications were disaggregated.
In-hospital mortality rate was slightly higher in the normal-weight group than in the other BMI groups, though differences were not significant (normal versus overweight OR: 1.17, 95% CI: 0.70-1.95, p = 0.554; normal versus obese OR: 1.09, 95% CI: 0.59-2.00, p = 0.789) (Fig. 2). There was no statistical difference between observed and
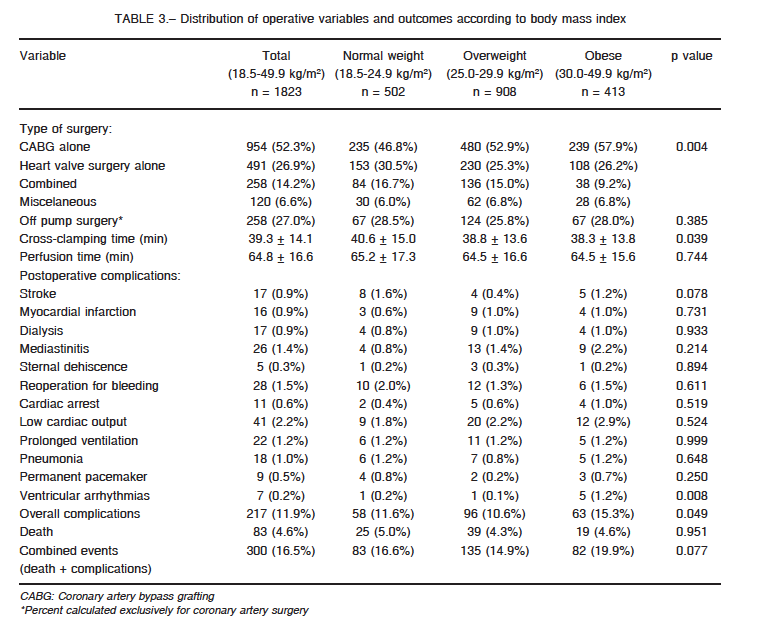
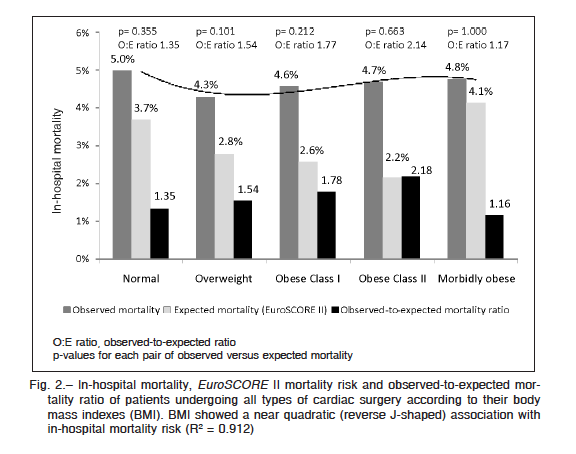
expected mortality for each individual BMI group; nevertheless, the expected mortality risk according to EuroSCORE II was significantly different among BMI groups (ANOVA F = 2.98, p = 0.018; Tukey’s test p = 0.046 for post hoc comparison between normal and overweight groups), with the normal-weight group showing the highest expected risk.
After adjusting by propensity score, a total of 806 patients for normal versus overweight comparison and 460 patients for normal versus obese comparison showed no systematic differences in the distribution of covariates.
Differences in in-hospital mortality rates were preserved, and complications rates became similar after propensity score-matched normal versus overweight groups were compared (mortality rate 4.2% versus 3.5%, OR: 1.22, 95% CI: 0.59-2.52, p = 0.583, and complications 8.4% versus 8.4%, OR: 1.00, 95% CI: 0.61-1.64, p = 1.000). Conversely, when comparing normal versus obese groups, differences in in-hospital mortality and complications rates were preserved after propensity score matching (mortality rate 3.5% versus 2.2%, OR: 1.62, 95% CI: 0.52-5.03, p = 0.399, and complications 6.5% versus 11.7%, OR: 0.52, 95% CI: 0.27-1.01, p = 0.052).
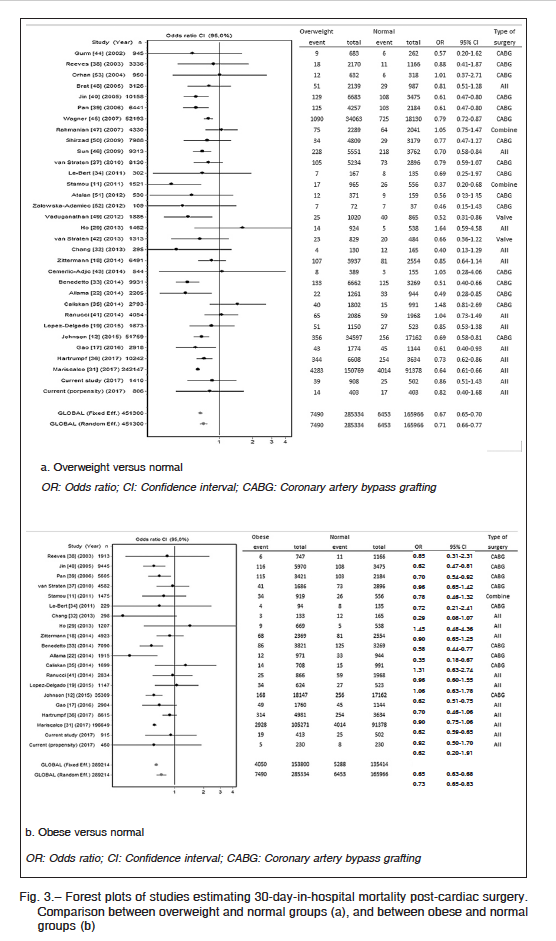
Out of 4410 initial independent references obtained through various search strategies comprising cardiac surgery and obesity, 30 eligible cohort observational studies were identified and included in the meta-analysis11, 12, 17-19, 22, 29, 31-53. When the data from our study before and after propensity score matching were included, the final meta-analysis population comprised 451 300 patients for the normal/overweight comparison (32 studies), and 289 214 patients for the normal/obese comparison (20 studies). The meta-analysis demonstrated the obesity paradox. Compared with overweight patients, the random observed global OR was 0.71 (95% CI, 0.66-0.77) for normal-weight individuals (Fig. 3.a), whereas compared with obese patients, the random observed global OR was 0.73 (95% CI, 0.65-0.83) for normal-weight patients (Fig. 3.b). Funnel plots revealed no evidence of publication bias in both mortality comparisons (Begg test Z = 0.60, p = 0.549 for overweight versus normal groups, and Z = 0.29, p = 0.770 for obese versus normal groups). Between-study heterogeneity was statistically significant in the analysis of both overweight versus normal-weight patients (I. = 61.0%, Q = 62.0, p = 0.0008) and in obese versus normal-weight patients (I. = 74.4%, Q = 44.3, p = 0.0009).
Discussion
The initial unadjusted comparison of in-hospital mortality rates after cardiac surgery between the different BMI groups revealed the incipient reverse J-shaped distribution described in the obesity paradoxical effect, with overweight and class I obese patients showing the lowest mortalities. Nevertheless, the higher mortality rate found in patients with normal BMI can be easily explained by a greater expected risk according to EuroSCORE II. This expected risk was significantly higher than that predicted for the
other BMI groups, and even the observed-to-expected mortality ratio of the normal BMI cohort was closer to one. Therefore, this observation plus outcomes obtained from the propensity score analysis helped to question a clear obesity paradoxical effect on mortality when contrasting matched data of normal and overweight groups. Nonetheless, after propensity score analysis, obese patients presented a lower mortality rate compared with normal patients, but a higher complication rate. In short, relative to non-obese patients, overweight and obese individuals showed comparable or lower in-hospital mortality rates after cardiac surgery. On the contrary, the overall complication rates were similar in overweight and higher in obese patients compared with normal-weight individuals.
Evaluation relative to previous research becomes difficult because some studies bring together overweight and normal-weight patients in a single set of data20, 21, 23, 25, 28, 30, and adjustment by confounders was rarely done. The analysis of 4172 patients from the ARIAM registry21 demonstrated that after adjusting for severity and perfusion time, obese patients had mortality rate, complication rate, and length-of-stay similar to non-obese patients (BMI < 30 kg/m.). Ho el al.29 did not observe any “obesity paradox” in mortality rate assessment after adjusting data for the principal confounders. In a short series of 637 patients, obesity did not increase in-hospital mortality; however, it increased pulmonary and gastrointestinal complications after adjusting for age, sex, and comorbidities30. Conversely, in a cohort analysis with propensity score matching of 2440 patients, Stamou el al.11 communicated that overweight patients had a lower operative mortality than normal BMI patients (OR: 0.4, 95% CI: 0.2-0.9), whereas obese individuals had a comparable risk with respect to normal-weight patients.
As in other studies12, 19, 22, we found that overweight and obese patients were younger and with higher rates of male sex and diabetes compared with normal-weight patients. However, the higher rates of heart failure, pulmonary hypertension and valve endocarditis found in normal-weight patients had not been previously observed or considered.
Some considerations must be taken into account to evaluate the obesity paradox effect. Firstly, a normal BMI in a healthy person might be protective in a public health setting in which mortality is assessed in the long-term54. By contrast, an overweight or obese BMI might be protective in critical illnesses when comorbidities are frequent because mortality is high and is assessed in the short-term rather than years55-57. It is important to consider additional sources of bias for the “obesity paradox” phenomenon. Obese patients consistently undergo revascularization surgical procedures at a younger age than their non-obese counterparts and, consequently, may present with lower risk coronary anatomy58. Outcomes of the present study were consistent with this last observation, since obese patients were significantly younger, and coronary surgery was more common. On the other hand, the paradox may be due to selection bias if only a subgroup of the “healthiest” obese patients were selected for cardiac surgery59-60.
The present systematic review of observational studies suggested that overweight and obesity were associated with a neutral or beneficial effect on all-cause mortality after cardiac surgery. Meanwhile, pooled analysis of the 32 studies in the meta-analysis demonstrated a definite protective effect of overweight and obesity in general, on 30-day-in-hospital mortality rates post-cardiac surgery. Though moderate to high statistical heterogeneity was found in the analyses of overweight or obese versus normal-weight patients, nearly all studies reported a neutral or protective effect of higher BMI levels on mortality, providing supportive evidence that the summary effect sizes were the product of consistent results. Nevertheless, the pooled effect size found in the meta-analysis should be considered small (OR > 0.66)61.
Previously, two other meta-analyses reported similar outcomes. Oreopoulos et al.62 analyzed the effect of BMI only after coronary artery bypass grafting in 12 observational studies (nearly 75 000 patients). After coronary surgery, both overweight and obese patients had lower in-hospital mortality risks compared with normal-weight individuals (OR: 0.70, 95% CI: 0.63-0.77 and OR: 0.63, 95% CI: 0.56-0.71, respectively). Recently, Mariscalco et al.31 studied approximately 558 000 patients undergoing all types of cardiac surgery in 26 observational studies. They reported lower in-hospital mortality in overweight (OR: 0.79, 95% CI: 0.76-0.83), obese class I (OR: 0.81, 95% CI: 0.76-0.86) and obese class II (OR: 0.83; 95% CI: 0.74-0.94) patients relative to normal-weight individuals.
This study has some limitations. Since in most patients, BMI was calculated from self-reported weight and height, a systematic bias may arise when comparing with BMI calculated from objectively measured data. Nevertheless, in large studies54, self-reported and measured BMI differed on average by only 3%, with a 95% correlation coefficient between them. It is possible that overweight or obese patients with a more severe profile of comorbidities and considered at high risk for a cardiac operation were excluded from surgery. Isolated BMI used as a marker of obesity also has limitations, since other aspects of body composition such as visceral fat distribution were not explored in this study. Finally, early reductions in mortality observed in obese patients may not be sustained in the mid- and long-term.
In conclusion, this study showed that overweight and obese patients had similar or slightly lower in-hospital mortality rates after cardiac surgery compared with normal-weight individuals. Conversely, postoperative complication rates systematically increased with higher BMI levels. Most observational studies included in the systematic review showed that overweight and obese patients had at least the same mortality rate as normal-weight patients, or even a lower death risk. Pooled-data of the meta-analysis provided evidence on the association between higher BMI levels and a lower all-cause in-hospital mortality rate after cardiac surgery.
Conflict of interests: None to declare
Bibliografía
1. Logue J, Murray HM, Welsh P, et al. Obesity is associated with fatal coronary heart disease independently of traditional risk factors and deprivation. Heart 2011; 97: 564-8.
2. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet 2014; 383: 970-83.
3. De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. J Obes 2013; 2013: 291546.
4. Zhang X, Lerman LO. Obesity and renovascular disease. Am J Physiol Renal Physiol 2015; 309: F273-9.
5. Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther 2013; 35: A18-32.
6. Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006; 355: 763-78.
7. McAuley PA, Blair SN. Obesity paradoxes. J Sports Sci 2011; 29: 773-82.
8. Chen Z, Yang G, Offer A, et al. Body mass index and mortality in China: a 15-year prospective study of 220 000 men. Int J Epidemiol 2012; 41: 472-81.
9. Amundson DE, Djurkovic S, Matwiyoff GN. The obesity paradox. Crit Care Clin 2010; 26: 583-96.
10. Klasen J, Junger A, Hartmann B, et al. Increased body mass index and peri-operative risk in patients undergoing non-cardiac surgery. Obes Surg 2004; 14: 275-81.
11. Stamou SC, Nussbaum M, Stiegel RM, et al. Effect of body mass index on outcomes after cardiac surgery: is there an obesity paradox? Ann Thorac Surg 2011; 91: 42-7.
12. Johnson AP, Parlow JL, Whitehead M, Xu J, Rohland S, Milne B. Body Mass Index, and mortality following cardiac surgery in Ontario, Canada. J Am Heart Assoc 2015; 4: e0022140.
13. Parlow JL, Ahn R, Milne B. Obesity is a risk factor for failure of “fast track” extubation following coronary artery bypass surgery. Can J Anesth 2006; 53: 288-94.
14. Engel AM, McDonough S, Smith JM. Does an obese body mass index affect hospital outcomes after coronary artery bypass graft surgery? Ann Thorac Surg 2009; 88: 1793-800.
15. Tyson GH, Rodriguez E, Elci OC, et al. Cardiac procedures in patients with a body mass index exceeding 45: outcomes and long-term results. Ann Thorac Surg 2007; 84: 3-9.
16. Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg 2012; 41: 734-44.
17. Gao M, Sun J, Young N, et al. Impact of Body Mass Index on outcomes in cardiac surgery. J Cardiothorac Vasc Anesth 2016; 30: 1308-16.
18. Zittermann A, Becker T, Gummert JF, Börgermann J. Body mass index, cardiac surgery and clinical outcome. A single-center experience with 9125 patients. Nutr Metab Cardiovasc Dis 2014; 24: 168-75.
19. Lopez-Delgado JC, Esteve F, Manez R, et al. The influence of body mass index on outcomes in patients undergoing cardiac surgery: does the obesity paradox really exist? PLoS One 2015; 10: e0118858.
20. Baslaim G, Bashore J, Alhoroub K. Impact of obesity on early outcomes after cardiac surgery: experience in a Saudi Arabian center. Ann Thorac Cardiovasc Surg 2008; 14: 369-75.
21. Curiel-Balsera E, Muñoz-Bono J, Rivera-Fernández R, Benitez-Parejo N, Hinojosa-Pérez R, Reina-Toral A; en representación de los investigadores del proyecto ARIAM de cirugía cardiaca de adultos de Andalucía. Consequences of obesity in outcomes after cardiac surgery. Analysis of ARIAM registry. Med Clin (Barc) 2013; 141: 100-5.
22. Allama A, Ibrahim I, Abdallah A, et al. Effect of body mass index on early clinical outcomes after cardiac surgery. Asian Cardiovasc Thorac Ann 2014; 22: 667-73.
23. Yap CH, Mohajeri M, Yii M. Obesity and early complications after cardiac surgery. Med J Aust 2007; 186: 350-4.
24. Rehman SM, Elzain O, Mitchell J, et al. Risk factors for mediastinitis following cardiac surgery: the importance of managing obesity. J Hosp Infect 2014; 88: 96-102.
25. Dişcigil G, Ozkisacik EA, Badak MI, Güneş T, Dişcigil B. Obesity and open-heart surgery in a developing country. Anadolu Kardiyol Derg 2008; 8: 22-6.
26. Moulton MJ, Creswell LL, Mackey ME, Cox JL, Rosenbloom M. Obesity is not a risk factor for significant adverse outcomes after cardiac surgery. Circulation 1996; 94 (9 Suppl): II87-92.
27. Rockx MA, Fox SA, Stitt LW, et al. Is obesity a predictor of mortality, morbidity and readmission after cardiac surgery? Can J Surg 2004; 47: 34-8.
28. Virani SS, Nambi V, Lee VV, et al. Obesity: an independent predictor of in-hospital postoperative renal insufficiency among patients undergoing cardiac surgery? Tex Heart Inst J 2009; 36: 540-5.
29. Ho KM, Bertenshaw C, Same S, et al. Differential associations between body mass index and outcomes after elective adult cardiac surgery: a linked data cohort study. Anaesth Intensive Care 2013; 41: 573-83.
30. Demir A, Aydınlı B, Güçlü ÇY, et al. Obesity and postoperative early complications in open heart surgery. J Anesth 2012; 26: 702-10.
31. Mariscalco G, Wozniak MJ, Dawson AG, et al. Body Mass Index and mortality among adults undergoing cardiac surgery: A Nationwide Study With a Systematic Review and Meta-Analysis. Circulation 2017; 135: 850-863.
32. Chang CH, Lee FY, Wang CC, et al. An obesity paradox of Asian body mass index after cardiac surgery: arterial oxygenations in duration of mechanic ventilation. Scientific World Journal 2013; 2013: 426097
33. Benedetto U, Danese C, Codispoti M. Obesity paradox in coronary artery bypass grafting: myth or reality? J Thorac Cardiovasc Surg 2014; 147: 1517-23.
34. Le-Bert G, Santana O, Pineda AM, Zamora C, Lamas GA, Lamelas J. The obesity paradox in elderly obese patients undergoing coronary artery bypass surgery. Interact Cardiovasc Thorac Surg 2011; 13: 124-7.
35. Caliskan E, Güsewell S, Seifert B, et al. Does body mass index impact the early outcome of surgical revascularization? A comparison between off-pump and on-pump coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2014; 19: 749-55.
36. Hartrumpf M, Kuehnel RU, Albes JM. The obesity paradox is still there: a risk analysis of over 15 000 cardiosurgical patients based on body mass index. Interact Cardiovasc Thorac Surg 2017; 25: 18-24.
37. van Straten AH, Bramer S, Soliman Hamad MA, et al. Effect of body mass index on early and late mortality after coronary artery bypass grafting. Ann Thorac Surg 2010; 89: 30-7.
38. Reeves BC, Ascione R, Chamberlain MH, Angelini GD. Effect of body mass index on early outcomes in patients undergoing coronary artery bypass surgery. J Am Coll Cardiol 2003; 42: 668-76.
39. Pan W, Hindler K, Lee VV, Vaughn WK, Collard CD. Obesity in diabetic patients undergoing coronary artery bypass graft surgery is associated with increased postoperative morbidity. Anesthesiology 2006; 104: 441-7.
40. Jin R, Grunkemeier GL, Furnary AP, Handy JR Jr. Is obesity a risk factor for mortality in coronary artery bypass surgery? Circulation 2005; 111: 3359-65.
41. Ranucci M, Ballotta A, La Rovere MT, Castelvecchio S; Surgical and Clinical Outcome Research (SCORE) Group. Postoperative hypoxia and length of intensive care unit stay after cardiac surgery: the underweight paradox? PLoS One 2014; 9: e93992.
42. van Straten AH, Safari M, Ozdemir HI, Elenbaas TW, Hamad MA. Does the body mass index predict mortality after isolated aortic valve replacement? J Heart Valve Dis 2013; 22: 608-14.
43. Cemerlić-Adjić N, Pavlović K, Jevtić M, Velicki R, Kostovski S, Velicki L. The impact ofn early mortality after coronary artery bypass grafting. Vojnosanit Pregl 2014; 71: 27-32.
44. Gurm HS, Whitlow PL, Kip KE; BARI Investigators. The impact of body mass index on short- and long-term outcomes in patients undergoing coronary revascularization: insights from the Bypass Angioplasty Revascularization Investigation (BARI). J Am Coll Cardiol 2002; 39: 834-40.
45. Wagner BD, Grunwald GK, Rumsfeld JS, et al. Relationship of body mass index with outcomes after coronary artery bypass graft surgery. Ann Thorac Surg 2007; 84: 10-6.
46. Sun X, Hill PC, Bafi AS, Garcia JM, Haile E, Corso PJ, Boyce SW. Is cardiac surgery safe in extremely obese patients (body mass index 50 or greater)? Ann Thorac Surg 2009; 87: 540-6.
47. Rahmanian PB, Adams DH, Castillo JG, Chikwe J, Bodian CA, Filsoufi F. Impact of body mass index on early outcome and late survival in patients undergoing coronary artery bypass grafting or valve surgery or both. Am J Cardiol 2007; 100: 1702-8.
48. Brát R, Kolek M. Is obesity a real risk factor in cardiosurgical procedures? Rozhl Chir 2005; 84: 342-5.
49. Vaduganathan M, Lee R, Beckham AJ, et al. Relation of body mass index to late survival after valvular heart surgery. Am J Cardiol 2012; 110: 1667-78.
50. Shirzad M, Karimi A, Armadi SH, et al. Effects of body mass index on early outcome of coronary artery bypass surgery. Minerva Chir 2009; 64: 17-23.
51. Atalan N, Fazlioğulları O, Kunt AT, et al. Effect of body mass index on early morbidity and mortality after isolated coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2012; 26: 813-7.
52. Zalewska-Adamiec M, Bachorzewska-Gajewska H, Malyszko J, et al. Impact of diabetes on mortality and complications after coronary artery by-pass graft operation in patients with left main coronary artery disease. Adv Med Sci 2014; 59: 250-5.
53. Orhan G, Biçer Y, Aka SA, et al. Coronary artery bypass graft operations can be performed safely in obese patients. Eur J Cardiothorac Surg 2004; 25: 212-7.
54. Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016; 388: 776-86.
55. Hogue CW Jr, Stearns JD, Colantuoni E, et al. The impact of obesity on outcomes after critical illness: a meta-analysis. Intensive Care Med 2009; 35: 1152-70.
56. Oliveros H, Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity 2008; 16: 515-21.
57. Pepper DJ, Sun J, Welsh J, Cui X, Suffredini AF, Eichacker PQ. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: a systematic review and meta-analysis. Crit Care 2016; 20: 181.
58. Rubishtein R, Halon DA, Jaffe R, Shahla J, Lewis BS. Relation between obesity and severity of coronary artery disease in patients undergoing coronary angiography. Am J Cardiol 2006; 87: 1277-90.
59. Yancy WS Jr, Olsen MK, Curtis LH, et al. Variations in coronary procedure utilization depending on body mass index. Arch Int Med 2005; 165: 1381-7.
60. King KM, Southern DA, Cornuz J, Knudtson ML, Ghali WA. Elevated body mass index and access to coronary revascularization following cardiac catheterization. Can J Cardiol 2006; 22(Suppl D): 290.
61. Sullivan GM, Feinn R. Using Effect Size – or Why the P value is not enough. J Grad Med Educ 2012; 4: 279-82.
62. Oreopoulos A, Padwal R, Norris CM, Mullen JC, Pretorius V, Kalantar-Zadeh K. Effect of obesity on short- and long-term mortality postcoronary revascularization: A meta-analysis. Obesity 2008; 16: 442-50.
